.png)
Introducing Air Nurses x ParaFlight: In-Flight Medical Care, Redefined
Expert Care, In Flight
At ParaFlight, we are proud to offer an exclusive service that goes beyond traditional private jet charters by partnering with Air Nurses, a concierge flight nursing service designed specifically for luxury medical transport in private aviation. Together, we provide a seamless and elevated in-flight medical experience, ensuring that comfort and medical expertise go hand-in-hand throughout the entire journey.
.png)
Who Is Air Nurses?
Air Nurses is a luxury concierge medical service offering board-certified flight nurses who provide comprehensive in-flight medical care. Founded by Ericka Essington BSN, RN, NRP, CFRN, FP-C, CMTE with over 15 years of experience in critical care transport and aviation medicine. Air Nurses have set the bar for medical oversight in private aviation. With Air Nurses, you have a team of elite, aviation-experienced professionals who are solely dedicated to providing medical care and peace of mind during the flight. They come on board your flight as additional crew, seamlessly integrating with your team to ensure continuous medical oversight throughout the journey.
Whether assisting with post-surgical recovery, managing chronic conditions, supporting elderly and pediatric travelers, or offering care for individuals with cognitive needs or those requiring additional support during recovery and wellness transitions, Air Nurses delivers a calm, capable presence onboard, ensuring seamless continuity and comfort from the moment you leave the ground to your final destination.
How Air Nurses Elevates ParaFlight’s Services
• In-Flight Medical Expertise: Air Nurses provide expert medical care aboard private jets, ensuring clients receive real-time monitoring, medication management, and mobility assistance, all while maintaining the highest standard of care. This clinical oversight guarantees that clients with complex medical needs travel safely and comfortably.
• Tailored Medical Solutions: Air Nurses offer customized solutions for each individual flight. From personalized medications and medical equipment to specific care protocols, Air Nurses ensure that every need is anticipated and addressed before departure, allowing clients to travel with confidence.
• Door-to-Destination Care: Air Nurses provide seamless, door-to-destination care, from bedside-to-aircraft transfers to arrival at the destination, ensuring continuous care throughout the entire journey.
• Coordinated Care: Air Nurses work in tandem with ParaFlight and any relevant physicians, family offices, and destination teams, making sure the journey is as smooth and efficient as possible. This seamless coordination enhances the overall experience, ensuring that all aspects of the trip, medical and logistical.are perfectly aligned.
• Luxury and Precision: By adding Air Nurses to ParaFlight’s suite of services, we deliver not only luxury aviation but also peace of mind for travelers with medical needs. This seamless integration of luxury aviation and medical care provides clients with a solution that meets both their comfort and health needs.
A New Class of Medically Supported Travel
Air Nurses and ParaFlight are elevating the standard for in-flight medical care, offering a refined alternative built specifically for private aviation. Every mission combines clinical expertise with seamless charter execution, delivering calm, comfort, and continuity at altitude.
Let’s Build the Mission Around You
For tailored itineraries and onboard medical support, contact our team 24/7:
📧 info@paraflight.aero
📞 1-844-538-1911 (Immediate Assistance)
Explore All Resources
Browse our full archive of travel guides, educational content, case studies, and service breakdowns.

The Critical Role of Private Jet Mobilization in Disaster Zones: Delivering Rapid Relief When Every Second Counts
When natural disasters strike, the difference between life and death often comes down to response time. While commercial aviation systems buckle under the pressure of mass evacuations and infrastructure damage, private jets emerge as critical lifelines, delivering personnel, supplies, and hope to devastated communities. This comprehensive analysis explores how private aviation serves as an essential component of disaster relief operations, transforming emergency response through speed, flexibility, and precision.
The Speed Imperative: Why Private Jets Lead Emergency Response
In disaster scenarios, time is of the essence and can make the difference between life and death. Traditional commercial aviation faces significant constraints during emergencies. Airports close, scheduled flights cancel, and passenger volumes overwhelm infrastructure. Private jets, however, operate with remarkable agility that proves invaluable during crisis situations.
Private jets are not fixed to a specific schedule and can take to the skies in any direction with very little notice. This flexibility becomes crucial when disaster zones require immediate attention. While commercial carriers may need days to restore service, private aircraft can launch relief missions within hours of a disaster declaration.
Typically, jet charter brokers work with air carriers to arrange last-minute flights for take off in as little as four hours from the time you call. This rapid deployment capability represents a critical advantage when every moment counts in life-or-death situations.
Strategic Access: Reaching the Unreachable
One of the most significant advantages private jets bring to disaster relief is their ability to access compromised infrastructure. A rapid response thanks to their ability to operate from regional airports and rural airfields with short runways. Their flexibility allows them to reach remote areas faster than any other transportation method.
During major disasters, primary airports often become overwhelmed or damaged. Airports are often closed immediately following one of these events; non-governmental relief organizations (NGOs) can enter, but standard private jet charters can't. These airports reopen once emergency supplies have arrived and a relief effort is underway. This creates a critical window where private aviation serves as a bridge between the immediate aftermath and broader recovery efforts.
The operational flexibility of private jets proves particularly valuable during hurricane recovery operations. Recovery efforts in the aftermath of a hurricane can be immense and require close coordination at both the federal and the state levels. The airspace around the recovery efforts have high levels of aviation activity, including small airplanes, helicopters, and drones.
Medical Evacuation: Life-Saving Mobility
Medical evacuations represent one of the most critical applications of private aviation in disaster relief. When a ground ambulance is not an option because of remoteness or distance and flying commercially is not viable for a patient's needs, a medical evacuation aircraft with medical equipment and trained staff is likely the best or only option.
In emergencies where local healthcare facilities are overwhelmed or inaccessible, private jets can transport critically ill or injured individuals to specialized medical centers equipped to provide life-saving treatment. The ability to customize aircraft interiors with advanced medical equipment and trained medical personnel ensures that patients receive timely care during transport.
Private aviation's role in medical emergencies encompasses several critical scenarios:
- Emergency Repatriation: After having received medical care in a local health facility, people may require the use of an air ambulance or private jet to repatriate them to their home country for further healthcare and recovery
- Organ Transport: Time-critical organ transplant missions where commercial aviation cannot meet the narrow time windows required
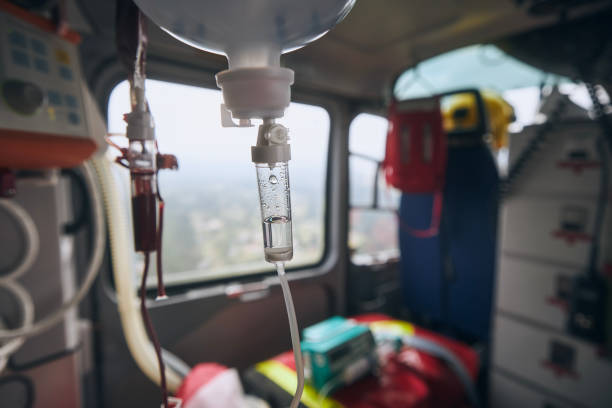
- Specialized Medical Support: Some people need critical help, such as a ventilator or an intravenous drip during transportation. While this is impossible on an airliner, it is relatively straightforward to accommodate on a private jet
Logistical Superiority: Delivering Critical Resources
Beyond passenger transport, private jets serve as essential cargo platforms for disaster relief operations. The logistical value of private jets is that they can deliver emergency supplies and evacuate people who are injured or in danger. Their cargo capabilities become particularly valuable when delivering specialized equipment to remote or damaged locations.
During the COVID-19 pandemic, private jets were vital in delivering personal protective equipment (PPE) and vaccines to urgently needed areas. This experience demonstrated how private aviation could rapidly adapt to serve emergency supply chain needs.
Recent disaster response efforts showcase this versatility across multiple emergency scenarios, from hurricane relief operations delivering supplies to affected regions, to international aid missions transporting essential medical supplies and PPE to areas in urgent need.
Evacuation Operations: Precision Under Pressure
Mass evacuation scenarios demonstrate private aviation's unique value proposition. With roadways often becoming impassable and commercial flights grounded, evacuation flights offer a rapid escape route for those in the path of a storm.
Private charter services have access to an extensive network of private charter planes, which allows coordination of emergency flights and evacuations anywhere in the world, and for any number of passengers, often with just four hour's notice.
Case studies from recent hurricanes illustrate this capability in action. When Hurricane Maria hit Puerto Rico, emergency response teams made around 17 evacuation flights out of the region within a matter of days, while also helping arrange many flights for NGOs and transporting rescue dogs left behind in the aftermath of natural disasters.
Regulatory Coordination and Safety Protocols
The integration of private aviation into disaster response requires sophisticated coordination with federal authorities. At the request of local authorities or law enforcement, the Federal Aviation Administration can issue Temporary Flight Restrictions (TFRs) to ensure safety for aircraft conducting Hurricane rescue and recovery activities. These TFRs do not ban aircraft, including drones, from providing disaster relief and recovery assistance.
Relief operations, including civilian and volunteer operations, may access the restricted airspace if they are coordinated with emergency responders. This regulatory framework ensures that private aviation operations complement rather than complicate official relief efforts.
The FEMA Coordination Framework
Understanding how private aviation integrates with federal disaster response provides insight into the broader emergency management ecosystem. FEMA has staff deployed to disaster operations across the country and U.S. territories in response to requests for federal assistance. FEMA maintains a cadre of more than 4,000 reservists to deploy to disaster zones, in addition to thousands of surge capacity force members from other federal agencies who can be called to respond if needed.
Private aviation serves as a force multiplier for these federal capabilities, particularly when government resources become stretched across multiple disaster zones or when specialized transport requirements exceed federal capacity.
Economic Impact and Cost Considerations
The economic dimensions of private jet disaster relief operations reflect both the value and challenges of this critical service. While emergency aviation services command premium pricing due to their specialized nature and urgent deployment requirements, the cost-benefit analysis often strongly favors rapid private aviation response.
During major hurricane operations, the economic impact becomes evident through the variety of charter requests spanning mass evacuation flights, urgent transportation due to travel disruption, flights to reach affected islands, and relief cargo flights with humanitarian aid shipments.
Technological Integration and Future Capabilities
As emergency response technology evolves, private aviation continues to adapt and integrate new capabilities. Modern aircraft feature advanced navigation systems, satellite communications, and weather radar that enhance their effectiveness in challenging disaster environments.
The future of disaster relief aviation may include enhanced drone coordination, artificial intelligence-assisted flight planning, and improved integration with emergency management systems. However, these technologies remain in development phases and are not yet standard capabilities across the private aviation fleet.
The ParaFlight Advantage: Expert-Driven Emergency Response
In the high-stakes world of disaster relief aviation, the quality of coordination and expertise can determine mission success. ParaFlight's concierge, expert-driven model provides critical advantages during emergency scenarios. Our approach emphasizes partnership with FAA-certified operators, ensuring that every mission meets the highest safety and regulatory standards.
Our team's deep understanding of emergency aviation requirements enables rapid response coordination without compromising safety or regulatory compliance. By working exclusively with certified operators, we eliminate the operational uncertainties that can compromise relief missions during critical moments.
The expert-driven approach proves particularly valuable when navigating the complex regulatory environment surrounding disaster relief operations. Our specialists understand TFR requirements, coordination protocols with emergency management agencies, and the operational constraints that can affect mission success.
Global Reach and Rapid Deployment
Private aviation's global reach enables international disaster response capabilities that extend far beyond domestic operations. With an international network of offices across six continents, private aviation services can provide local knowledge on a global scale. This international capability becomes crucial during major disasters that require cross-border coordination and resource mobilization.
The global nature of modern disaster response often requires rapid deployment across multiple time zones and regulatory jurisdictions. Private aviation's flexibility and international operational capabilities make it an essential component of coordinated international relief efforts.
Training and Preparedness Protocols
The effectiveness of private aviation in disaster relief depends heavily on preparedness and specialized training. Experience is very important during a disaster. Abnormal conditions during relief efforts call for experienced pilots who are instrument rated and current. This emphasis on experience reflects the challenging conditions that disaster relief pilots often encounter.
Specialized disaster relief operations require understanding of:
- Emergency landing procedures at compromised airports
- Coordination with military and government aircraft
- Navigation in areas with damaged infrastructure
- Fuel management when supply chains are disrupted
Often fuel supplies have not been replenished or are in short supply. If fuel is available, there may be long waits to receive it or cash may be required to pay.
Operational Considerations During Disasters
General aviation can be a lifeline in times of natural or national disaster. Volunteer pilots can help with search & rescue efforts or aerial assessment of damage. They may transport medical and emergency relief staff, deliver critical medical and relief supplies to affected areas, or relocate survivors or evacuees.
The coordination of disaster relief flights requires careful attention to operational details. Supply deliveries should not be conducted without checking in with relief flight charities, as dropping supplies on the ramp of a disaster area airport complicates the relief effort and can hinder ground operations. Coordination with relief flight charities is essential for any supply or volunteer needs.
Looking Forward: Enhancing Disaster Relief Aviation
The role of private jets in disaster relief continues to evolve as both technology and emergency management practices advance. Several trends are shaping the future of this critical capability:
Enhanced Integration: Improved coordination systems between private aviation and federal emergency management agencies will streamline response times and improve operational efficiency.
Specialized Equipment: Development of modular aircraft configurations that can rapidly convert between passenger evacuation, medical transport, and cargo delivery roles.
Predictive Deployment: Advanced weather modeling and disaster prediction may enable more proactive positioning of relief aircraft before disasters strike.
International Standards: Development of international protocols for cross-border disaster relief aviation operations to facilitate rapid global response.
Conclusion: An Indispensable Emergency Resource
Private jet mobilization in disaster zones represents far more than luxury aviation. It embodies a critical emergency response capability that saves lives, delivers hope, and accelerates recovery. The unique combination of speed, flexibility, and precision that private aviation brings to disaster relief operations makes it an indispensable component of modern emergency management.
As climate change increases the frequency and severity of natural disasters, the importance of private aviation in relief operations will only grow. The investment in maintaining this capability through proper regulation, operator certification, and coordination protocols represents an investment in community resilience and emergency preparedness.
For communities facing the devastating impact of natural disasters, private jets often represent the difference between isolation and connection, between delayed aid and immediate relief, between despair and hope. In an era where disasters strike with increasing unpredictability and severity, private aviation stands ready as a vital lifeline, connecting those in need with the resources, medical care, and safety that can make all the difference when every second counts.
References:

Maximizing Roadshow Success: The Strategic Integration of Ground Transportation and Private Aviation Services
In today's fast-paced business environment, executive teams and investment professionals increasingly rely on roadshows to build relationships, secure funding, and expand market presence. The success of these critical business initiatives often hinges on seamless logistics that maximize time efficiency while maintaining the highest levels of professional presentation. The Private Jet Charter Services Market is expected to reach USD 16.38 billion in 2025 and grow at a CAGR of 7.95% to reach USD 24.02 billion by 2030, reflecting the growing demand for integrated travel solutions that streamline complex multi-destination itineraries.
The Evolution of Business Travel Integration
Current Market Landscape
The private jet industry is experiencing significant growth in 2024, surpassing pre-pandemic levels. As of mid-May 2024, private flying has surged, surpassing pre-pandemic levels seen in 2019 by an impressive 32.1%. This remarkable growth underscores a fundamental shift in how executives approach business travel, prioritizing efficiency and control over traditional commercial alternatives. The industry was worth $21.24 billion in 2024 and is expected to grow to $24.28 billion in 2025, driven largely by increased business travel needs, with 77% of business travelers said they took one to five trips in 2023, but 7% took more than 10 trips.
The modern roadshow presents unique logistical challenges that require sophisticated coordination between air and ground transportation services. Unlike routine business travel, roadshows demand precision timing, multiple daily meetings across different cities, and the ability to adapt quickly to schedule changes while maintaining executive-level service standards.
The Integration Imperative
The seamless integration of private aviation and ground transportation defines the ultimate VIP travel experience. This integration becomes particularly crucial during roadshows where effective communication between private aviation and ground transportation providers is essential. Coordination ensures that all aspects of the journey are synchronized, from flight arrival times to vehicle readiness. Dedicated concierge services often manage this intricate process, ensuring that all logistics are handled with precision.
The Roadshow Challenge: Why Traditional Travel Falls Short
Time Constraints and Efficiency Demands
Investment banking roadshows, corporate presentations, and business development tours operate under extreme time pressure. A typical roadshow might involve visiting five to seven cities in a single week, with multiple meetings scheduled in each location. This intensive schedule leaves no margin for delays, missed connections, or logistical failures.
Traditional commercial aviation simply cannot accommodate these demands. Flight schedules remain inflexible, security procedures consume valuable time, and connections between airports and meeting venues often require multiple transportation modes. VIP ground services include precise coordination to ensure that vehicles are ready and waiting upon arrival. This level of service minimizes wait times and guarantees that the transition from aircraft to ground is both smooth and timely.
The Cost of Inefficiency
For high-stakes roadshows, time inefficiency translates directly to financial impact. Investment banking teams conducting IPO roadshows, for example, operate within narrow market windows where delays can affect valuation and timing. Similarly, corporate acquisition teams must maintain momentum during due diligence processes and stakeholder presentations.
High-net-worth individuals are becoming more plentiful across the globe, with their wealth reaching $86.8 trillion in 2023. People with this kind of money can afford private flights, recognizing that the premium paid for integrated services delivers measurable returns in terms of deal success and relationship building.
ParaFlight's Comprehensive Concierge Approach
Beyond Transportation: Complete Journey Management
With ParaFlight, private travel is as simple as saying 'Let's go.' Whether for a last-minute board meeting, an international site visit, or a well-earned retreat, we handle every detail with precision and care. An aviation solution built for business leaders and teams who demand efficiency, reliability, and flexibility.
This comprehensive approach recognizes that successful roadshows require more than point-to-point transportation. They demand orchestrated logistics that account for ground transportation coordination, meeting venue accessibility, catering requirements, and real-time schedule adjustments.
Expert-Driven Coordination
Our unmatched safety record, certified excellence, and tailored concierge services set us apart from competitors. ParaFlight's concierge team brings specialized expertise in roadshow logistics, understanding the unique demands of different business verticals and the critical success factors for multi-city presentations.
The expert-driven model ensures that each roadshow receives customized planning based on specific industry requirements, client preferences, and strategic objectives. This personalization extends beyond basic transportation to encompass venue selection assistance, local market intelligence, and contingency planning for weather or schedule disruptions.
Strategic Integration of Services
Ground Transportation Coordination
Whether you require a reliable private car service for an airport transfer or a multi-vehicle charter for a financial roadshow, every ground transportation reservation managed to ensure a safe and seamless ground travel experience. Effective roadshow logistics require sophisticated ground transportation networks that can accommodate varying group sizes, security requirements, and timing constraints.
Professional transportation coordination services understand the demanding and critical nature of investment banking and financial roadshows. Their reputation as leaders in executive transportation for the financial sector allows them to maintain preferred status with many of the largest, most recognizable investment banks and firms around the globe.
Real-Time Coordination and Monitoring
Modern roadshow logistics leverage advanced technology platforms for real-time coordination. Professional roadshow coordinators watch trips in real-time, ensuring chauffeurs are where they are supposed to be, precisely when they are supposed to be there. Real-time coordination teams make itinerary changes as they are communicated, acting as liaisons between passengers, travel arrangers, chauffeurs, and dispatch.
This level of coordination ensures that ground transportation aligns perfectly with aircraft arrival times, accounting for weather delays, air traffic control holds, and other variables that could disrupt carefully planned schedules.
FBO Integration and Private Terminal Services
VIP ground transportation is another service provided by FBOs to ensure a smooth transition between the airport and the passenger's final destination. This can include luxury car services, limousines, or even helicopters, depending on the client's preferences and requirements. The FBO staff will ensure that the transportation arrangements are made seamlessly, allowing passengers to proceed swiftly and comfortably to their next destination.
FBOs are designed to balance efficiency with unparalleled comfort. While they offer quick boarding and expedited customs procedures to streamline your experience, their luxurious lounges and crew facilities emphasize private aviation's focus on personal comfort and flexibility. In this regard, the aircraft often waits for you to make sure that your schedule remains uniquely yours.
Technology-Enabled Efficiency
Digital Platform Integration
The integration of digital technologies is enhancing the connectivity between air and ground services. Real-time updates, automated scheduling, and intelligent routing are streamlining the travel experience, ensuring that VIPs enjoy an uninterrupted journey.
Advanced booking platforms now enable seamless coordination between aviation and ground transportation services. These systems provide real-time visibility into flight progress, ground traffic conditions, and venue accessibility, allowing for proactive adjustments that maintain schedule integrity.
Predictive Analytics and Route Optimization
Modern roadshow logistics increasingly rely on predictive analytics to optimize routing and timing. By analyzing historical traffic patterns, weather data, and venue accessibility factors, logistics coordinators can identify potential bottlenecks and develop contingency strategies before they impact schedule execution.
Route planning coordinators work with event planners to map out routes between locations, ensuring all participants can navigate efficiently between meetings while accounting for local traffic patterns and infrastructure limitations.
Quantifying the Efficiency Advantage
Time Savings and Productivity Gains
The integration of ground transportation and private aviation services delivers measurable time savings that translate directly to business value. Traditional commercial travel for a five-city roadshow might require 15-20 hours of transit time, compared to 8-12 hours with integrated private services. This 40-50% time reduction allows for additional meetings, more thorough preparation time, and reduced executive fatigue.
Market Access and Flexibility
Access thousands of private airports, bypassing delays and congestion. Whether heading to a boardroom, a remote site, or a life-saving mission, the most direct route is always our priority. Private aviation provides access to over 5,000 airports in the United States alone, compared to fewer than 500 served by commercial airlines. This expanded access enables roadshow teams to reach secondary markets and business centers that would be difficult or impossible to visit efficiently using commercial transportation.
ROI Considerations
While integrated private travel services command premium pricing, the return on investment often proves compelling for high-stakes roadshows. Investment banking teams conducting IPO roadshows, for example, may generate hundreds of millions in fees from successful offerings. In this context, the incremental cost of integrated transportation services represents a minimal investment relative to potential returns.
Industry-Specific Applications
Investment Banking and Capital Markets
Financial services roadshows operate under unique constraints that make integrated transportation essential. Long-term client relationships develop when service providers demonstrate consistent reliability in high-pressure environments, with some corporate access roadshow needs spanning over 12 years of reliable service.
Investment banking roadshows require coordination with institutional investors across multiple time zones, often with same-day schedule changes based on market conditions or investor availability. The ability to adjust routing and timing in real-time becomes crucial for maximizing investor meetings and maintaining deal momentum.
Corporate Development and M&A
Merger and acquisition activities frequently involve multi-city due diligence processes where executive teams must visit facilities, meet with management teams, and conduct stakeholder presentations across diverse geographic locations. These processes often operate under strict confidentiality requirements and tight timing constraints driven by regulatory deadlines or competitive dynamics.
Technology Sector Roadshows
Technology companies conducting investor relations roadshows face unique challenges related to international market access and rapid schedule changes. Silicon Valley-based companies, for example, frequently need to reach Asian and European markets within compressed timeframes, requiring seamless coordination between transpacific flights and local ground transportation networks.
Sustainability and Future Considerations
Environmental Responsibility
The push towards sustainability is influencing both private aviation and ground transportation. More eco-friendly aircraft and hybrid vehicles are becoming prevalent, reflecting a growing commitment to reducing the environmental impact of luxury travel.
Modern roadshow logistics increasingly incorporate sustainability considerations without compromising efficiency. This includes optimizing routing to reduce overall travel distances, utilizing sustainable aviation fuel options where available, and coordinating with ground transportation providers who maintain hybrid or electric vehicle fleets.
Technological Innovation
Artificial intelligence is playing an increasing role in predictive aircraft maintenance, helping operators identify service needs before they cause disruptions, delays, or worse, safety issues. These technological advances will continue to enhance roadshow reliability by reducing the likelihood of equipment failures or unexpected delays.
Emerging technologies such as advanced air mobility and electric vertical takeoff and landing aircraft may further revolutionize roadshow logistics by enabling point-to-point transportation that bypasses traditional airport infrastructure entirely.
Best Practices for Roadshow Planning
Pre-Planning and Route Optimization
Successful roadshow integration begins with comprehensive pre-planning that considers all logistical variables. This includes analyzing venue locations relative to airport facilities, identifying optimal aircraft positioning strategies, and establishing contingency plans for weather or mechanical delays.
Established roadshow coordinators provide knowledge and expertise to seamlessly handle all requirements, whether organizing a chauffeur-driven roadshow in Boston, New York, or London. The roadshow booking process is streamlined for convenience, with simple itinerary email submissions confirmed within minutes, including chauffeur contact details provided the day before each roadshow. All itineraries are meticulously checked, traveling times confirmed, and updates quickly actioned and reconfirmed.
Communication Protocols
Effective roadshow logistics require established communication protocols that enable real-time coordination between aviation crews, ground transportation providers, and executive travelers. This includes designated points of contact, escalation procedures for schedule changes, and backup communication methods for international travel.
Quality Assurance and Vendor Management
Experienced team members with access to all itinerary details remain available 24/7. Each trip includes multiple quality control checks. Rigorous vendor management ensures that all service providers meet established standards for reliability, safety, and service quality.
Measuring Success and Continuous Improvement
Key Performance Indicators
Successful roadshow logistics require measurable performance indicators that track both efficiency and client satisfaction. These typically include on-time performance metrics, schedule adherence rates, and client feedback scores. Advanced logistics providers maintain detailed performance databases that enable continuous improvement and trend analysis.
Client Feedback and Service Evolution
You guys provide such amazingly stellar service and follow up. I am not sure I could do my job if I wasn't backed by the amazing Commonwealth Team. I have used a lot of companies over the years, but since I started using Commonwealth, they are the only call I ever have to make. Long-term client relationships enable service providers to refine their offerings based on real-world experience and evolving business requirements.
The Future of Integrated Roadshow Logistics
Market Evolution and Growth Projections
Projections by The Business Research Company indicate that the global market for private jet rental services will grow from $21.24 billion in 2024 to $24.28 billion in 2025, at a compound annual growth rate (CAGR) of 14.3%. This growth is attributed to increased demand for flexible, customized travel solutions, as well as an increase in the number of affluent individuals and business travelers seeking alternatives to commercial flights.
This growth trajectory reflects not only increased demand for private aviation services but also the growing recognition of integrated logistics as a competitive differentiator for business success.
Emerging Service Models
Fractional ownership and jet sharing are gaining ground, making private aviation more accessible and flexible. These models help reduce costs while enjoying the exclusive benefits of private jet travel. These evolving business models may create new opportunities for integrated roadshow services that serve mid-market clients who previously relied on commercial aviation.
Conclusion: The Strategic Imperative for Integration
The integration of ground transportation and private aviation services represents more than a luxury convenience; it constitutes a strategic business tool that enables executives to maximize the effectiveness of high-stakes roadshows. We don't just move jets—we move people, business, and opportunities.
In an increasingly competitive business environment, the ability to execute flawless multi-city presentations while maintaining schedule flexibility and executive productivity provides measurable competitive advantages. Companies that recognize this strategic value and invest in integrated transportation solutions position themselves to capture opportunities that might otherwise be compromised by logistical limitations.
ParaFlight's expert-driven concierge model exemplifies the evolution toward comprehensive service integration that addresses every aspect of roadshow logistics. Our concierge team ensures proper handling and supervision throughout the journey, delivering the reliability and flexibility that modern business demands.
As we approach 2025, the private aviation market is poised for further expansion, supported by emerging trends and challenges that will shape its trajectory. The integration of ground and air transportation services will become increasingly sophisticated. Organizations that embrace these integrated solutions today will be best positioned to capitalize on future business opportunities while maintaining the operational efficiency that drives sustainable competitive advantage.
The future of roadshow logistics lies not in simply moving executives from point A to point B, but in creating seamless, technology-enabled experiences that maximize every moment of valuable executive time while ensuring flawless execution of critical business initiatives. Through expert coordination, real-time monitoring, and comprehensive service integration, ParaFlight delivers the roadshow efficiency that drives business success in today's dynamic marketplace.
References

How Private Aviation Enhances Productivity During Roadshow Travel: The Ultimate Executive Advantage
In today's hyper-competitive business landscape, time is the most valuable currency for executives conducting roadshows. Whether you're pitching to investors, visiting multiple client sites, or conducting strategic business meetings across different markets, the efficiency of your travel directly impacts your success. Private aviation has emerged as the definitive solution for maximizing productivity during roadshow travel, offering unparalleled advantages that transform how business leaders approach multi-destination trips.
The Roadshow Travel Challenge: Why Commercial Aviation Falls Short
Corporate roadshows present unique travel challenges that commercial aviation simply cannot address effectively. Nearly nine in 10 (87%) business travelers lose at least one hour of productivity due to stress from their journey, with almost one in two C-level executives, business owners and senior managers losing four to eight hours of productive time during a business trip.
The traditional approach to roadshow travel using commercial airlines creates a cascade of inefficiencies:
- Fixed scheduling constraints that force business agendas around airline timetables
- Multiple connections requiring extended layovers in major hub cities
- Limited destination accessibility to secondary markets and remote business locations
- Security delays and boarding processes that consume valuable executive time
- Lack of privacy preventing confidential business discussions during travel
For executives managing complex roadshow itineraries across multiple cities, these limitations translate into lost opportunities and diminished productivity.
The Private Aviation Advantage: Quantifying Productivity Gains
Time Savings That Transform Business Operations
The productivity advantages of private aviation during roadshow travel are both measurable and substantial. Private jet travelers save an average of 2 hours (127 minutes) per flight over commercial aviation. For executives conducting roadshows involving multiple destinations, these time savings compound dramatically.
These efficiencies can save between 2 to 5 hours per flight. For those flying 400 hours a year, this translates to saving 800 to 2,000 hours annually, equivalent to up to 2.5 months of extra time each year.
Enhanced Market Accessibility
One of the most significant advantages for roadshow travel is private aviation's superior market accessibility. Private jets can access about 5000 airports nationwide, which is about 4500 more than commercial jets! This expanded reach enables executives to:
- Visit manufacturing facilities in secondary markets
- Reach remote business locations without commercial service
- Access regional financial centers efficiently
- Conduct same-day multi-city visits that would be impossible via commercial aviation
Productivity During Flight
The productivity differential between private and commercial aviation becomes even more pronounced when examining in-flight work capabilities. Only 42% said they were able to get work done during a commercial flight. However, 63% said they felt effective and productive on private flights.
This 21% productivity increase during flight time represents significant value for executives who need to prepare for meetings, conduct confidential calls, or strategize with team members while traveling.
Strategic Business Applications: Roadshow Success Stories
Multi-Destination Efficiency
Consider a typical investment roadshow scenario where executives need to visit institutional investors across multiple cities. A team of four executives traveling commercially from New York to visit three Midwestern manufacturing facilities would typically require 3-4 days. Between advance arrival requirements, connection delays, limited direct flights to smaller markets, and inefficient ground transportation between facilities, productive time gets compressed into small windows. The same itinerary via private aviation often collapses into a single day, visiting all three facilities and returning home for dinner.
Flexibility for Dynamic Schedules
Roadshow itineraries frequently require last-minute adjustments based on client availability, market conditions, or strategic opportunities. Flexibility is cited as the primary reason to use private business aircraft as opposed to commercial flights. Fifty-two percent noted that regular commercial airlines could not accommodate their scheduling needs.
This scheduling flexibility proves invaluable during roadshows when:
- Meeting times shift due to client availability
- Additional prospects request last-minute meetings
- Weather or market conditions require route modifications
- Success in one market creates immediate opportunities in adjacent regions
Privacy and Confidentiality
Roadshow travel often involves sensitive business discussions, financial data review, and strategic planning. Private aviation provides the confidential environment necessary for these high-stakes conversations. Executives can make use of the travel time to work, hold meetings, or prepare for important presentations, ensuring that their time is put to optimal use. The privacy and security provided by private aircraft also protect sensitive information and maintain confidentiality.
Financial Justification: The ROI of Private Aviation for Roadshows
Executive Time Valuation
The financial case for private aviation during roadshows becomes compelling when examining executive time valuation. For an executive whose time is valued at $1,000 per hour, saving 800 to 2,000 hours annually equates to a potential value of $800,000 to $2,000,000.
For roadshow-specific scenarios, consider these calculations:
- Traditional 3-day roadshow via commercial aviation: 24 executive hours traveling
- Same roadshow via private aviation: 8 executive hours traveling
- Time savings: 16 hours per executive
- Team of 4 executives: 64 hours saved
- **At $500/hour executive value**: $32,000 in recovered productivity per roadshow
Competitive Advantage Quantification
Companies are increasingly relying on business jets to enhance productivity, particularly when it comes to accessing secondary cities or remote sites that lack efficient commercial airline service. This enhanced accessibility creates tangible competitive advantages:
- First-mover advantage in emerging markets
- Deeper client relationships through more frequent face-to-face interactions
- Faster deal execution through compressed negotiation timelines
- Enhanced due diligence capabilities for acquisition opportunities
ParaFlight's Concierge Approach: Redefining Executive Travel Excellence
In the private aviation landscape, ParaFlight has distinguished itself through its expert-driven, concierge model that specifically addresses the complex needs of roadshow travel. Unlike transactional booking platforms, ParaFlight's approach centers on comprehensive travel orchestration that ensures every aspect of your roadshow contributes to business success.
Expert Flight Coordination
ParaFlight's team of aviation professionals brings decades of experience in orchestrating complex multi-destination itineraries. With ParaFlight, private travel is as simple as saying 'Let's go.' Whether for a last-minute board meeting, an international site visit, or a well-earned retreat, we handle every detail with precision and care. An aviation solution built for business leaders and teams who demand efficiency, reliability, and flexibility.
This level of service proves invaluable during roadshows when itineraries require:
- Real-time route optimization based on client availability
- Aircraft selection tailored to passenger count and range requirements
- Ground transportation coordination at each destination
- Contingency planning for weather or operational challenges
Global Accessibility and Range
ParaFlight's comprehensive aircraft portfolio ensures optimal solutions for any roadshow requirement. Unrestricted global mobility. Direct access to financial hubs, remote business sites, and premier destinations because business and life don't wait.
Whether your roadshow requires:
- Light jets for regional multi-city tours
- Mid-size aircraft for coast-to-coast investor meetings
- Heavy jets for international market expansion initiatives
- Ultra-long-range aircraft for global roadshow campaigns
ParaFlight's expert team matches aircraft capabilities precisely to mission requirements, ensuring maximum efficiency and cost-effectiveness.
Operational Excellence and Safety
ParaFlight's commitment to operational excellence extends beyond convenience to encompass the safety protocols essential for executive travel. YOUR SAFETY. OUR PRIORITY. From quick business hops to intercontinental journeys, we source the right aircraft to fit your itinerary and priorities.
Industry Statistics: The Growing Adoption of Business Aviation
The business aviation industry has experienced remarkable growth, driven largely by productivity demands from executive travelers. As per Statista, the global business jet market exceeded $24 billion in value in 2020. Projections indicate that by 2028, it's expected to approach $37 billion.
This growth reflects increasing recognition of private aviation's value proposition for business productivity. Growing market size: The private jet market has grown steadily over the years, fueled by increasing demand for private jet travel from high-net-worth individuals, corporate clients, and luxury travellers.
Business Travel Productivity Trends
Recent research confirms what executives have long understood about business travel's productivity impact. According to a new study from the company, six in ten travelers feel more creative and productive when traveling for business. However, this productivity boost is amplified significantly when travel occurs via private aviation rather than commercial flights.
The efficiency gains are particularly pronounced for face-to-face business interactions. CWT said its research also shows that six in ten travelers are most productive when working face-to-face and collaborating with colleagues, as opposed to working alone (30%) or remotely (14%).
Maximizing Roadshow Success: Best Practices with Private Aviation
Strategic Route Planning
Successful roadshow execution via private aviation requires strategic route optimization that considers:
- Geographic clustering of meetings to minimize flight time
- Market prioritization based on business opportunity size
- Timing coordination to maximize face-to-face interaction quality
- Contingency routing for weather or operational challenges
Team Coordination and Logistics
In a scenario where your executive team needs to visit multiple cities in different areas of the country for meetings, private travel can provide incredible cost-saving advantages. Rather than flying commercial and taking multiple days to travel back and forth, private travel can reduce this trip to a single day. Instead of paying for multiple nights at hotels and multiple meals for the entire team, all meetings can happen in one day.
Technology Integration
Modern roadshow success requires seamless technology integration throughout the travel experience. ParaFlight's comprehensive approach ensures:
- Mobile connectivity for real-time communication during travel
- Ground transportation coordination via integrated logistics
- Meeting preparation facilitation through private cabin environments
- Real-time itinerary adjustments based on business developments
The Future of Roadshow Travel: Sustainability and Innovation
Environmental Considerations
As corporate sustainability initiatives gain prominence, private aviation operators are responding with innovative solutions. Sustainable aviation fuel is crucial in reducing the carbon footprint of business aviation. As the industry aims for sustainability, the usage of sustainable aviation fuel is expected to increase, impacting the overall business aviation statistics.
Forward-thinking companies are incorporating sustainability metrics into their roadshow travel decisions, seeking operators committed to environmental responsibility without compromising efficiency.
Conclusion: Transforming Roadshow Success Through Private Aviation
The evidence is unequivocal: private aviation transforms roadshow travel from a necessary business expense into a strategic competitive advantage. The productivity gains ranging from time savings and enhanced accessibility to confidential meeting capabilities and scheduling flexibility create measurable value that far exceeds the investment for most executive travel scenarios.
For organizations serious about maximizing roadshow effectiveness, the question isn't whether private aviation provides value, but rather how quickly they can implement this strategic advantage. The calculus is clear: When properly integrated into corporate travel strategy, private aviation transforms from perceived extravagance to measurable competitive advantage. The question isn't whether your organization can afford private air travel; it's whether your strategic initiatives can afford the opportunity costs of commercial alternatives.
ParaFlight's concierge, expert-driven model represents the evolution of private aviation services, moving beyond simple aircraft provision to comprehensive travel orchestration that ensures every aspect of your roadshow contributes to business success. In an era where competitive advantage often comes down to execution speed and market access, private aviation isn't just a luxury; it's a business imperative.
The next time your organization plans a roadshow, consider not just the cost of private aviation, but the cost of not maximizing every opportunity your roadshow presents. With the right aviation partner and strategic approach, your roadshow travel can become a powerful driver of business growth rather than merely a logistical necessity.
References
- ProfileTree - Business Aviation Statistics
- NBAA - Why Use Aircraft for Business Travel
- Business Traveller - Business Travel Productivity Report
- Scoop Market - Business Jets Statistics 2025
- ParaFlight - Executive Flights and Travel

Fastest MEDEVAC Flight Coordination in Phoenix: How Expert Planning Saves Lives Through Rapid Response Aviation
When medical emergencies strike in the Phoenix metropolitan area, every second counts toward connecting patients with life-saving care. Medical evacuation (MEDEVAC) services represent the critical bridge between emergency scenes and specialized medical facilities, requiring precise coordination with FAA-certified operators who conduct helicopter air ambulance operations under strict Part 135 requirements. Phoenix, Arizona's fifth-largest city with over 1.7 million residents, relies on sophisticated flight coordination expertise to ensure the fastest possible emergency medical response times across the sprawling Sonoran Desert landscape.
At ParaFlight, we specialize in coordinating these critical medical transportation services by connecting families and medical facilities with qualified, FAA-certified air medical operators throughout the Phoenix region. Our expert-driven approach ensures seamless coordination when minutes matter most.
Understanding MEDEVAC Flight Coordination Excellence in Phoenix
Medical evacuation flight coordination involves orchestrating a complex network of emergency medical services, FAA Part 135 certified aviation operators, hospital systems, and communication centers working in perfect synchronization. In Phoenix, this intricate coordination system serves not only the metropolitan area but extends across rural Arizona, where ground transportation to major medical facilities can take hours.
The Phoenix MEDEVAC system operates under strict Federal Aviation Administration (FAA) guidelines, with aircraft using the "MEDEVAC" designation to receive priority handling from air traffic controllers. This coordination extends to Phoenix Sky Harbor International Airport, one of the busiest airports in the United States handling over 44 million passengers annually.
The Critical Timeline: Understanding Emergency Response
The first 60 minutes after traumatic injury has been termed the "golden hour," a concept that has been taught and practiced for more than 3 decades. However, recent scientific evidence suggests the "golden hour" concept is pervasive despite little evidence to support it. Research indicates that median emergency response times from 911 call to hospital arrival average 36.3 minutes across diverse North American locations.
In Phoenix's urban sprawl covering over 500 square miles, ground ambulances face significant challenges including traffic congestion, distance to trauma centers, and harsh desert conditions. Medical evacuation operations provide rapid response capabilities, with helicopters offering agility for urban areas and rugged terrain access.
Phoenix's MEDEVAC Infrastructure and Certified Operators
Working with FAA-Certified MEDEVAC Providers
Phoenix benefits from multiple FAA-certified MEDEVAC operators, each maintaining strategically positioned aircraft throughout the metropolitan area. ParaFlight coordinates with these certified operators to ensure optimal coverage and response capabilities.
These certified operators maintain aircraft equipped with advanced life support equipment and staffed by experienced flight nurses and paramedics who meet stringent certification requirements including nationally registered EMT-P status, extensive critical care experience, and current ACLS, ITLS, CPR, and PALS certifications.
State-of-the-Art Medical Aircraft Standards
Modern MEDEVAC helicopters are specialized aircraft equipped with medical equipment and personnel to swiftly transport patients to hospitals or trauma centers. These FAA-certified aircraft feature:
- Advanced cardiac monitoring systems
- Ventilators and airway management tools
- Blood and medication storage capabilities
- Satellite communication systems for real-time medical consultation
- Night vision capabilities for 24/7 operations
- GPS navigation systems with hospital landing zone databases
The Phoenix Advantage: Geographic and Operational Benefits
Optimal Flying Conditions for Emergency Operations
Phoenix's desert climate provides significant advantages for MEDEVAC operations. With over 300 sunny days annually and minimal precipitation, weather-related flight restrictions are less common compared to other major metropolitan areas. FAA regulations require certified operators to obtain weather reports from approved sources within 15 nautical miles of airports for safe operations.
Strategic Hospital Network Integration
Phoenix's trauma care system includes several Level I trauma centers equipped with helipads designed for rapid patient transfer. The city's medical infrastructure supports seamless integration between air and ground emergency services through coordinated planning.
Advanced Communication and Expert Coordination Systems
Unified Emergency Response Through Expert Planning
Phoenix's MEDEVAC coordination relies on sophisticated communication systems connecting multiple agencies through expert coordination services like ParaFlight:
911 Emergency Dispatch Centers immediately assess situations requiring air medical transport, considering factors such as injury severity, location accessibility, and hospital capacity.
Flight Operations Centers coordinate with FAA-certified operators for aircraft deployment, weather monitoring, and air traffic control communications to ensure optimal flight paths and minimal response times.
Hospital Communication Networks provide real-time updates on trauma bay availability, specialist coverage, and landing zone conditions.
Technology Integration in Coordination Services
Modern MEDEVAC coordination utilizes advanced technology including:
- Automated vehicle location (AVL) systems tracking emergency response assets
- Computer-aided dispatch (CAD) systems providing instant access to medical facility capabilities
- Weather monitoring systems providing real-time atmospheric conditions
- GPS-based navigation with obstacle databases for safe low-altitude flight operations
Response Time Performance and Industry Standards
According to the Association of Air Medical Services (AAMS), established in 1980, the organization is dedicated to advancing transport medicine through advocacy, education, and research to ensure high-quality, life-saving care. Industry benchmarks suggest optimal response targets, though actual performance varies by location and circumstances.
Estimated optimal MEDEVAC response goals include:
- Dispatch to airborne: Under 8 minutes (industry estimate)
- Scene response time: 15-20 minutes for urban areas (estimated)
- Patient transport time: Minimized through strategic hospital selection
- Total response time: Under 30 minutes for most metropolitan emergencies (estimated)
Note: These are industry estimates and actual response times may vary based on numerous factors including weather, aircraft availability, and specific circumstances.
Challenges and Solutions in Desert MEDEVAC Operations
Environmental Considerations for Certified Operators
Operating MEDEVAC services in Phoenix's Sonoran Desert environment presents unique challenges for FAA-certified operators:
Temperature Extremes: Summer temperatures exceeding 120°F affect aircraft performance and require specialized procedures. FAA regulations require pilots to demonstrate familiarity with local flying areas through examination within 12 months.
Dust and Visibility: Desert dust storms (haboobs) can rapidly reduce visibility, requiring sophisticated weather monitoring and alternative transport protocols.
Terrain Obstacles: Phoenix's mountainous terrain requires specialized navigation capabilities and obstacle avoidance systems for safe operations.
Urban Aviation Coordination Challenges
Phoenix's rapid urban development creates ongoing coordination challenges:
Infrastructure Complexity: Extensive electrical infrastructure requires detailed mapping and specialized navigation for safe low-altitude operations.
Traffic Considerations: While helicopters avoid ground traffic, landing zone access coordination can be complicated by traffic patterns.
Community Integration: Balancing rapid response requirements with community considerations requires careful flight path planning.
Training and Certification Excellence Standards
Medical Crew Certification Requirements
Phoenix MEDEVAC operations maintain strict medical staffing standards, with flight nurses requiring critical care experience and advanced certifications, while flight paramedics need extensive advanced life support experience and specialized equipment training.
Transport nursing represents a unique and expanded role encompassing air and surface medical transport of critically ill and injured patients.
Pilot Certification Standards
MEDEVAC pilots must meet stringent FAA requirements including commercial or airline transport pilot licenses with instrument ratings, with dispatcher certifications preferred. Additional requirements typically include:
- Minimum flight hours with significant helicopter experience
- Instrument flight rating with night vision qualifications
- Mountain flying experience and desert operation familiarity
- Regular recurrent training in emergency procedures
Integration with Regional Emergency Systems Through Expert Coordination
Multi-State Coordination Capabilities
Phoenix's MEDEVAC system frequently requires coordination with neighboring states for specialized care transfers. Patients requiring treatment unavailable in Phoenix may need transport to facilities in California, Colorado, or Utah, requiring complex inter-state medical transport coordination expertise.
Rural Arizona Coverage Extension
Phoenix-based coordination services extend coverage throughout rural Arizona, where ground transport distances to trauma centers can exceed 200 miles. This coordination requires:
- Extended range capability planning
- Communication with remote landing zones
- Coordination with volunteer emergency services
- Weather monitoring across diverse geographic regions
Quality Assurance and Continuous Improvement
Performance Monitoring Systems
AAMS advocates on behalf of the medical transport community to ensure sustainability, increase medical quality and patient safety. Quality assurance programs include:
Response Time Analysis: Continuous monitoring of coordination efficiency and transport effectiveness.
Safety Management Systems: Comprehensive safety programs tracking incidents and implementing preventive measures.
Outcome Assessment: Following coordination effectiveness to improve future response planning.
Future Innovation in Coordination Technology
Phoenix MEDEVAC coordination services are preparing for emerging technologies:
Enhanced Communication Networks: Future 5G-enabled capabilities may provide improved connectivity between coordination centers and medical facilities.
Predictive Analytics: Data-driven systems for demand pattern prediction and optimal resource positioning are being developed.
Autonomous Systems Integration: Future autonomous flight systems may enhance safety and operational efficiency, though these remain in development phases.
Economic Impact and Community Benefits
Healthcare System Integration Benefits
Expert MEDEVAC coordination provides significant benefits to Phoenix's healthcare system:
- Improved emergency department efficiency through strategic patient distribution
- Enhanced trauma center utilization optimization
- Reduced coordination complexity for hospital staff
- Streamlined communication between multiple providers
Community Safety Enhancement
Professional MEDEVAC coordination services enhance overall community safety by ensuring rapid access to qualified, FAA-certified operators when emergencies occur. This coordination infrastructure supports Phoenix's continued growth and development.
Future Developments in Phoenix MEDEVAC Coordination
Emerging Technologies on the Horizon
Phoenix MEDEVAC coordination is monitoring technological advances for future integration:
Electric Aircraft Development: Research into electric MEDEVAC helicopters may offer reduced operating costs and environmental impact in the future.
Unmanned Systems Research: Development of drone technology for medical supply delivery and scene assessment remains in experimental phases.
AI-Enhanced Coordination: Artificial intelligence applications for coordination optimization are being researched, though not yet operationally deployed.
Expansion and Growth Planning
As Phoenix continues rapid population growth, coordination services are expanding:
- Enhanced coordination capabilities with additional certified operators
- Improved integration with emerging hospital systems
- Expanded coverage areas serving Arizona's growing population
- Advanced training and coordination capabilities
The ParaFlight Advantage: Expert-Driven MEDEVAC Coordination
Why Choose Professional Coordination Services
ParaFlight's expert-driven coordination model provides several key advantages:
Exclusive Partnership with FAA-Certified Operators: We work only with fully certified, compliant operators who meet the highest safety and operational standards.
24/7 Expert Coordination: Our experienced team provides round-the-clock coordination services, ensuring rapid response when emergencies occur.
Comprehensive Network Access: Through our established relationships with certified operators, we can coordinate the most appropriate aircraft and crew for each specific situation.
Regulatory Compliance Assurance: Our expertise ensures all coordinated flights meet FAA requirements and industry safety standards.
Our Coordination Process
When you contact ParaFlight for MEDEVAC coordination in Phoenix:
- Immediate Assessment: Our experts rapidly assess your specific medical transportation needs
- Operator Selection: We coordinate with the most appropriate FAA-certified operator for your situation
- Comprehensive Planning: We handle all coordination details including hospital communication, flight planning, and regulatory compliance
- Ongoing Support: We provide continuous coordination support throughout the entire transport process
Conclusion: Excellence in MEDEVAC Coordination When Lives Depend on It
Phoenix's MEDEVAC coordination success depends on expert planning, qualified operators, and sophisticated coordination systems working together seamlessly. By leveraging aviation assets and specialized medical expertise, these services facilitate timely access to critical care and enhance outcomes for patients in need through seamless coordination between healthcare providers, aviation professionals, and emergency responders.
ParaFlight's commitment to coordinating exclusively with FAA-certified operators ensures Phoenix residents and visitors receive optimal emergency medical transportation coordination when every second counts. Our expert-driven approach provides the professional coordination needed to navigate complex emergency medical transportation requirements while maintaining the highest safety and compliance standards.
Through ongoing relationship building with certified operators, continuous training, and system optimization, ParaFlight's coordination services continue setting standards for emergency medical aviation coordination nationwide, providing essential support for over two million metropolitan area residents and countless visitors to the Valley of the Sun.
When medical emergencies require immediate air transport coordination in Phoenix, trust ParaFlight's expertise to connect you with qualified, FAA-certified operators who can provide the life-saving transportation services you need.
References
- Federal Aviation Administration - Part 135 Helicopter Air Ambulance Operations
- Emergency Medical Services Intervals and Survival in Trauma - National Center for Biotechnology Information
- Association of Air Medical Services - Industry Leadership
- Federal Aviation Administration - MEDEVAC Flight Priority
- The Journalist's Resource - Emergency Medical Services Response Times
Booking a Medical Jet Charter in Philadelphia: Your Complete Guide with ParaFlight
When medical emergencies arise or specialized treatment requires travel, time becomes the most critical factor. For residents of Philadelphia and the surrounding areas, medical jet charter services provide life-saving transportation that bridges the gap between urgent medical needs and quality healthcare facilities. ParaFlight serves as your expert concierge partner, connecting you with FAA-certified operators who deliver hope, comfort, and critical care when every second counts.
Why Choose Medical Jet Charter Services?
Medical jet charter services have revolutionized emergency medical transportation and planned medical travel. Unlike commercial airlines, which have numerous restrictions and delays, medical jets are specifically equipped and staffed to handle patients requiring specialized care during transport.
The advantages of medical jet charter include immediate availability, specialized medical equipment, qualified medical personnel onboard, and the ability to fly directly to the nearest appropriate medical facility. Approximately 3% of all ambulance transports in the United States are performed by aeromedical assets, requiring over 300 air ambulance services, 1000 bases, and 1400 registered aircraft, according to the National Center for Biotechnology Information.
Philadelphia: A Strategic Location for Medical Air Transport
Philadelphia's position on the East Coast makes it an ideal hub for medical jet charter services. The city is home to some of the nation's most prestigious medical institutions, including the Hospital of the University of Pennsylvania, Jefferson Health, and Children's Hospital of Philadelphia (CHOP). However, patients often need transport to specialized facilities in other cities like Boston, New York, or even international destinations.
The Philadelphia region is served by multiple airports capable of handling medical jet operations, including Philadelphia International Airport (PHL), Northeast Philadelphia Airport (PNE), and Wings Field Airport (LOM). This network ensures that ParaFlight's partner operators can coordinate efficient medical flights regardless of weather conditions or air traffic constraints.
Types of Medical Jet Charter Services
Emergency Medical Transport
Emergency medical jet charter services are designed for critical situations where patients require immediate transport to specialized medical facilities. These flights operate 24/7 and can typically be airborne within 30-60 minutes of receiving a call. Aircraft operated by Part 135 certificate holders authorized by the Administrator to conduct helicopter air ambulance operations are equipped with advanced life support systems, ventilators, cardiac monitors, and other critical care equipment.
Emergency medical jets are staffed with certified flight nurses, paramedics, and when necessary, specialized physicians. Helicopters are ideal for transporting critical trauma patients because they are more effective in decreasing the time of transport to a trauma hospital. This is important because, for many critical trauma patients, the most important factor in decreasing mortality is getting them quickly to an operating room with a trauma surgeon.
Planned Medical Transport
Not all medical jet charter needs are emergencies. Planned medical transport serves patients who require specialized treatment at distant facilities but are stable enough for scheduled transport. This might include patients seeking treatment at renowned cancer centers, transplant facilities, or specialized pediatric hospitals.
Planned medical flights offer more flexibility in terms of timing and can often accommodate family members or caregivers. These flights are typically more cost-effective than emergency transports and allow for better coordination with receiving medical facilities.
Organ Transport
Philadelphia's medical institutions frequently participate in organ transplant programs, making rapid organ transport crucial. Medical jets equipped for organ transport maintain precise temperature and environmental controls necessary to preserve organs during transport. Time is especially critical in organ transport, as organs have limited viability outside the body.
International Medical Repatriation
For Philadelphia residents who become ill or injured while traveling abroad, international medical repatriation services provide transport back to familiar healthcare systems. These flights often require additional documentation, customs clearance, and coordination with international authorities.
ParaFlight: Your Expert Concierge Partner
ParaFlight distinguishes itself in the medical jet charter industry by serving as your dedicated concierge partner, connecting you exclusively with FAA-certified operators who maintain the highest standards of safety and medical care. Rather than owning aircraft or employing medical crews directly, ParaFlight leverages its extensive network of certified providers to ensure you receive the most appropriate and qualified medical transport services for your specific needs.
Our Partner Network
ParaFlight works exclusively with Part 135 certificate holders who maintain FAA certifications and medical personnel certified in advanced life support, flight medicine, and critical care transport. Our partner network includes operators whose teams comprise registered nurses with flight experience, paramedics trained in air medical protocols, and on-call physicians for complex cases. Each partner operator's crew members undergo continuous education and recertification to maintain the highest standards of medical care.
Fleet and Equipment Standards
Our partner operators maintain medical jets equipped with hospital-grade medical equipment including ventilators, defibrillators, IV pumps, cardiac monitors, and specialized equipment for pediatric and neonatal transport. Each aircraft maintains redundant systems to ensure continuous operation of critical medical devices throughout the flight.
The aircraft interiors are designed specifically for medical transport, with easy patient loading systems, adequate space for medical personnel to work, and secure mounting points for all medical equipment. Advanced communication systems allow medical teams to consult with receiving physicians during flight.
The Medical Jet Charter Process with ParaFlight
Initial Consultation
When you contact ParaFlight for medical jet charter services, our expert coordination team immediately begins the process of understanding your specific medical transport needs. This includes assessing the patient's medical condition, determining the urgency of transport, identifying the destination facility, and coordinating with our network of certified operators and medical teams at both origin and destination.
Medical Assessment and Partner Selection
Our team works with qualified medical professionals to review all available medical information and determine the appropriate level of care required during transport. This assessment helps us select the most qualified partner operator, determine staffing requirements, necessary equipment, and any special considerations for the flight.
Flight Planning and Coordination
ParaFlight's coordination team manages all aspects of the transport through our certified operator partners, including airport arrangements, customs and immigration requirements for international flights, ground ambulance coordination, and communication with receiving medical facilities.
Transport Execution
On the day of transport, our partner operator's ground team coordinates with the referring medical facility to ensure smooth patient transfer. The certified medical crew takes responsibility for the patient's care from departure to arrival, providing continuous monitoring and medical intervention as needed.
Cost Considerations and Insurance Coverage
Medical jet charter services represent a significant financial investment, with costs typically ranging from $15,000 to $50,000 for domestic flights within the United States, according to industry estimates. International flights can cost significantly more depending on distance, route complexity, and regulatory requirements.
Many insurance plans, including Medicare and private health insurance, provide coverage for medically necessary air transport when certain criteria are met. According to healthcare industry sources, air ambulance services must be deemed medically necessary and the patient must require services or equipment only available on air ambulances for coverage to apply.
ParaFlight works closely with insurance providers to verify coverage and ensure proper documentation for reimbursement. Our specialists understand the complex requirements for medical transport coverage and can help families navigate the insurance approval process.
Safety Standards and Regulatory Compliance
Safety is paramount in medical aviation. ParaFlight exclusively partners with operators who maintain 14 CFR Part 135 Air Carrier and Operator Certification from the Federal Aviation Administration (FAA), adhere to standards set by the Commission on Accreditation of Medical Transport Systems (CAMTS), a peer review organization dedicated to improving patient care and safety, and follow protocols established by the Association of Air Medical Services.
CAMTS is an independent, non-profit agency based in Sandy Springs, South Carolina, which audits and accredits fixed-wing, rotary wing, and surface medical transport services worldwide to a set of industry-established criteria. Our partner operators undergo rigorous training in medical flight operations, including specialized approaches to hospitals, weather minimums for medical flights, and coordination with air traffic control for priority handling.
Market Growth and Industry Statistics
The medical jet charter industry continues to expand significantly. The global air ambulance services market size was estimated at USD 14.6 billion in 2022 and is expected to grow at a CAGR of 10.7% from 2023 to 2030, according to Grand View Research. This growth reflects increasing recognition of the value these services provide in emergency medical care and planned medical transport.
Annually, critical care transport teams conduct approximately 300,000 rotor wing, 230,000 critical care ground, and 40,000 fixed wing transports, demonstrating the substantial demand for specialized medical transportation services.
Choosing the Right Medical Jet Charter Provider
When selecting a medical jet charter service in Philadelphia, consider several key factors:
Accreditation and Certifications
Look for providers who work exclusively with CAMTS-accredited operators and FAA Part 135 certified aircraft operators. These credentials ensure adherence to the highest safety and medical care standards.
Response Time and Coordination
Emergency medical situations require rapid response and expert coordination. Quality providers should be able to coordinate launches within one hour for emergency calls and provide realistic timeframes for planned transports through their network of certified operators.
Medical Capabilities
Ensure the provider can coordinate access to operators with your specific medical needs, whether that involves specialized equipment, particular medical personnel qualifications, or experience with your type of medical condition.
Insurance Coordination and Expert Guidance
Choose providers experienced in working with insurance companies and familiar with coverage requirements for medical transport. ParaFlight's concierge approach includes dedicated support throughout the insurance verification and approval process.
Future Innovations in Medical Air Transport
The medical aviation industry continues to evolve with advancing technology. Future innovations may include enhanced telemedicine capabilities for real-time consultation between flight crews and ground-based physicians, improved aircraft designs optimized for patient transport, and emerging technologies like autonomous systems that could enhance safety and efficiency in medical aviation operations.
While current operations rely on proven technologies and established protocols, the industry continues to explore how artificial intelligence and other emerging technologies might support improved patient outcomes and operational efficiency in the years ahead.
Conclusion
Medical jet charter services provide critical transportation for patients requiring specialized medical care or emergency transport. In Philadelphia, where world-class medical facilities attract patients from around the globe, medical air transport serves as a vital link between patients and the care they need.
ParaFlight combines expert coordination with access to the industry's most qualified, FAA-certified operators to provide comprehensive medical jet charter services. Our commitment to working exclusively with accredited providers ensures that patients and families receive the highest standards of safety, medical care, and customer service during challenging medical situations.
Whether facing a medical emergency requiring immediate transport or planning travel for specialized treatment, ParaFlight provides the expert concierge services Philadelphia residents can trust. Call ParaFlight today to learn how our medical air transport coordination services can serve your healthcare transportation needs through our network of certified operators.
References
- Loyd JW, Larsen T, Kuhl EA, et al. Aeromedical Transport. StatPearls [Internet]. 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK518986/
- Air Ambulance Services Market Size & Share Report. Grand View Research. 2023. Available from: https://www.grandviewresearch.com/industry-analysis/air-ambulance-services-market
- Federal Aviation Administration. 14 CFR Part 135 Air Carrier and Operator Certification. Available from: https://www.faa.gov/licenses_certificates/airline_certification/135_certification
- Commission on Accreditation of Medical Transport Systems. About CAMTS. Available from: https://www.camts.org/
Establishing Transport Statistics: Results From the Medevac Transport Statistics Survey. Air Medical Journal. 2019. Available from: https://www.airmedicaljournal.com/article/S1067-991X(18)30363-8/abstract

How ParaFlight Supports Boston-Area Hospitals with Urgent Medical Charters: Saving Lives Through Critical Air Transport
When medical emergencies require immediate specialized care, every minute can mean the difference between life and death. For Boston-area hospitals serving some of the nation's most complex cases, ParaFlight's expert concierge medical charter services provide the critical link between patients in need and the FAA-certified air transport operators who can deliver rapid, safe medical evacuation. As New England's trusted medical aviation concierge, ParaFlight specializes in coordinating urgent medical charters that help save lives across the region.
The Critical Demand for Medical Air Transport in Boston's Healthcare Network
Boston's world-renowned medical institutions serve not only the Greater Boston area's 4.9 million residents but also patients from across New England and beyond seeking specialized care. In FFY 2019, there were over 3.1 million ED visits in the Commonwealth, with many requiring transfer to specialized facilities for advanced treatments unavailable at their initial point of care.
The geographic challenges of New England create unique barriers for traditional ground transport. Rural areas of Massachusetts, New Hampshire, Vermont, and Maine can be hours away from the specialized trauma centers, cardiac facilities, and tertiary care hospitals concentrated in Boston. Weather conditions, particularly during harsh New England winters, can make ground transport dangerous or impossible, creating situations where air transport becomes the only viable option for patient survival.
Boston Children's Hospital alone cares for 60,000 patients with emergency medical needs each year, serving as one of the largest emergency/trauma centers in New England. Meanwhile, Boston Medical Center operates as the 11th busiest emergency department in the U.S., highlighting the tremendous volume of critical cases requiring specialized transport solutions.
ParaFlight's Expert Medical Charter Concierge Services
ParaFlight has established itself as New England's premier medical charter concierge service, specializing in connecting hospitals, medical facilities, and families with FAA-certified Part 135 operators who provide urgent medical air transport. Rather than owning aircraft or employing flight crews directly, ParaFlight leverages its deep industry expertise and extensive network of certified operators to ensure patients receive the fastest, safest medical transport available.
The ParaFlight Concierge Advantage
ParaFlight's expert-driven approach sets it apart in the medical charter industry:
Comprehensive Operator Vetting: ParaFlight maintains partnerships exclusively with FAA Part 135 certified operators who must obtain specific certifications for medical transport operations and Air Carrier Certificates with Operations Specifications from the FAA. This ensures every flight meets the highest federal safety standards.
24/7 Expert Coordination: ParaFlight's experienced medical aviation specialists provide round-the-clock coordination services, managing all aspects of medical charter arrangements from initial consultation through patient arrival at the destination facility.
Specialized Medical Equipment Oversight: Working with certified operators, ParaFlight ensures access to aircraft configured with state-of-the-art medical equipment comparable to intensive care units, including advanced life support systems, portable diagnostic equipment, and specialized patient transport systems.
Real-Time Flight Management: ParaFlight's expert coordinators monitor weather conditions, air traffic, and hospital capacity in real-time to optimize flight routing and timing for the most efficient patient transport possible.
Fleet Access and Medical Capabilities
Through its network of FAA-certified operators, ParaFlight provides access to medically-equipped aircraft specifically designed for critical patient transport. These aircraft feature:
- Advanced life support systems including ventilators and cardiac monitors
- Portable ultrasound and diagnostic equipment
- Emergency medication supplies and blood products storage
- Specialized patient transport stretchers and restraint systems
- Communication systems for real-time consultation with medical teams
The operator network includes turboprop aircraft capable of landing at smaller regional airports, ensuring accessibility to rural areas where ground transport times would be prohibitive. While ground ambulance transport from rural areas to Boston's major medical centers can exceed 90 minutes, air transport through ParaFlight's certified operators typically completes the same journey in 20-30 minutes.
Strategic Hospital Partnerships Across Boston
Massachusetts General Hospital Collaboration
Massachusetts General Hospital, consistently ranked among the nation's top hospitals, relies on ParaFlight's expert coordination services for urgent patient transfers requiring specialized services such as:
- Emergency cardiac surgery and interventional cardiology
- Advanced trauma care and neurosurgery
- Organ transplant procedures
- High-risk obstetrical care
The seamless coordination provided by ParaFlight's medical aviation experts has significantly improved door-to-treatment times for critical patients transferred from outlying facilities. In cardiac emergencies, these time savings directly translate to preserved heart muscle and improved long-term outcomes.
Brigham and Women's Hospital Integration
Brigham and Women's Hospital utilizes ParaFlight's concierge services primarily for complex cardiovascular cases and high-risk pregnancies. The hospital's maternal-fetal medicine program serves as a regional referral center, often requiring urgent transport of pregnant patients experiencing complications.
According to medical transport research, approximately 1.6 million patients are transferred between hospitals annually, with air transport reducing transfer times by an estimated 65% compared to ground ambulance services. This reduction is particularly crucial for time-sensitive conditions like placental abruption or fetal distress requiring immediate cesarean delivery.
Proven Impact on Patient Outcomes: Evidence-Based Results
The effectiveness of medical air transport coordinated through ParaFlight's expert services can be measured through concrete patient outcome improvements:
Survival Rate Improvements
A U.S. study using 2014 data found that after adjusting for age, Injury Severity Score, and gender, trauma patients who were transferred by helicopter were 57.0% less likely to die than those transferred by ground ambulance. This dramatic improvement in survival rates demonstrates the critical importance of rapid medical air transport for trauma patients.
Time-Critical Care Access
Helicopters are ideal for transporting critical trauma patients because they are more effective in decreasing the time of transport to a trauma hospital. This is important because, for many critical trauma patients, the most important factor in decreasing mortality is getting them quickly to an operating room with a trauma surgeon.
For stroke patients, research indicates that for every 30-minute reduction in transport time, the likelihood of good neurological outcome increases significantly. ParaFlight's coordination ensures that patients from rural New England locations reach Boston stroke centers in approximately 25 minutes compared to ground transport times that often exceed 90 minutes.
Enhanced Treatment Access
Patient outcomes are improved with use of trauma systems, which rely on well-trained crews and either fixed-wing aircraft or helicopters to rapidly manage and transport seriously ill patients from remote locations to the nearest appropriate trauma facility. In the United States, for example, the only way 28% of the population can access care at a trauma centre within the "golden hour" is by such services.
Navigating New England's Weather and Geographic Challenges
New England's unpredictable weather patterns create unique challenges for medical transport that ParaFlight's expert coordinators are specially trained to manage. During winter months, nor'easters and blizzard conditions can make ground transport impossible while still allowing properly equipped aircraft to operate safely.
ParaFlight's certified operator partners maintain:
- Pilots with specialized training for New England weather conditions
- Instrument flight rules (IFR) certification for low visibility operations
- Mountain flying capabilities for operations in Vermont and New Hampshire terrain
- Cold weather operations procedures and ice/snow landing techniques
The company's expert coordinators maintain advanced weather monitoring capabilities and work closely with Boston Logan International Airport and regional airports to ensure safe operations even during challenging weather conditions.
Advanced Communication and Technology Integration
Modern medical air transport relies heavily on seamless communication between aircraft, sending facilities, and receiving hospitals. ParaFlight's certified operator partners have invested in advanced communication technologies that enable:
Real-Time Medical Consultation
During transport, medical teams can maintain direct communication with physicians at both sending and receiving facilities, allowing for:
- Continuous monitoring updates and vital sign transmission
- Medication dosage adjustments based on patient response
- Preparation of receiving teams with specific equipment and specialists
- Complete documentation of all medical interventions during transport
Electronic Health Record Integration
Many of ParaFlight's operator partners utilize documentation systems that integrate with major hospital electronic health record platforms used by Boston-area hospitals, ensuring seamless information transfer and reducing the risk of medical errors during patient handoffs.
Economic Impact and Cost-Effectiveness
The economic implications of ParaFlight's medical charter coordination services extend beyond individual patient outcomes to broader healthcare system efficiency:
System-Wide Cost Benefits
While medical air transport involves higher upfront costs compared to ground ambulances, comprehensive cost-effectiveness studies demonstrate long-term savings through:
- Reduced hospital length of stay for transported patients
- Lower rates of complications requiring additional interventions
- Decreased likelihood of medical malpractice claims related to delayed care
- Improved hospital capacity utilization through faster patient turnover
Regional Healthcare Enhancement
ParaFlight's operations contribute to Boston's position as a regional medical hub, supporting the local economy through enhanced healthcare access and improved patient outcomes across New England.
Safety Standards and Regulatory Compliance
According to the National Transportation Safety Board (NTSB), commercial aviation under Part 135 has a substantially lower accident rate than general aviation. The comprehensive training requirements, maintenance standards, and operational procedures create multiple layers of safety protection.
FAA Part 135 Certification Requirements
All of ParaFlight's operator partners must meet stringent FAA Part 135 requirements, including:
- Medical Team Qualifications: Board-certified emergency physicians or critical care specialists, critical care nurses with air transport certification, and paramedics with advanced life support training
- Aviation Safety Standards: Pilots with minimum 3,000 hours of flight experience, instrument rating and commercial pilot certification, and annual safety training exceeding FAA requirements
- Aircraft Maintenance: Rigorous maintenance schedules and safety inspections that exceed standard aviation requirements
Continuous Safety Monitoring
Part 135 operators are subject to regular FAA oversight with routine inspections where FAA inspectors conduct regular inspections of operations, maintenance, and training programs, ensuring the highest safety standards are maintained.
Future Innovations in Medical Air Transport
ParaFlight continues to monitor emerging technologies and capabilities that may enhance medical air transport services in the future:
Emerging Medical Technologies
Future technological developments may include:
- Portable extracorporeal membrane oxygenation (ECMO) systems for the most critically ill patients
- Advanced point-of-care laboratory testing capabilities during transport
- Enhanced telemedicine platforms for specialist consultation during transport
- Drone technology for medical supply delivery in remote areas
Artificial Intelligence Applications
AI and machine learning may eventually enhance:
- Flight route optimization based on weather and air traffic patterns
- Predictive maintenance scheduling for medical equipment
- Real-time patient monitoring and alert systems
- Automated documentation and reporting systems
Addressing Industry Challenges
Despite its effectiveness, medical air transport faces ongoing challenges that ParaFlight addresses through innovative coordination solutions:
Weather-Related Contingencies
Weather conditions are an important consideration for air medical transport, and medical transport helicopters are often unable to accept flights when there is poor visibility. ParaFlight mitigates these challenges through:
- Multiple operator partnerships to provide backup coverage during weather events
- Advanced weather prediction systems for proactive planning
- Ground transport coordination for weather-related flight cancellations
- Flexible routing capabilities to avoid severe weather areas
Insurance and Coverage Coordination
Medical air transport costs can create financial barriers for patients and hospitals. ParaFlight works to address these concerns through:
- Insurance pre-authorization services to streamline coverage approval
- Transparent pricing coordination with operator partners
- Financial assistance program coordination for qualifying patients
- Advocacy for improved insurance coverage of medically necessary air transport
The Critical Role of Expert Medical Charter Coordination
There is a trend towards morbidity and mortality benefits of HEMS in time-critical trauma cases, but the data needed to improve the accuracy of dispatch criteria and better align urgent resources with the needs of patients are limited. This is where ParaFlight's expertise becomes invaluable.
ParaFlight's experienced coordinators understand the complex decision-making process involved in medical air transport, including:
- Patient acuity assessment and transport appropriateness
- Optimal aircraft selection based on medical needs and distance
- Weather and operational considerations
- Hospital capacity and receiving facility capabilities
- Insurance authorization and financial considerations
Conclusion: ParaFlight's Essential Role in Boston's Medical Transport Network
ParaFlight's expert medical charter concierge services have become an integral component of Boston's healthcare infrastructure, providing critical coordination that connects patients with life-saving air transport when they need it most. Through exclusive partnerships with FAA-certified Part 135 operators and a commitment to the highest safety standards, ParaFlight ensures that distance and time never become insurmountable barriers to life-saving medical treatment.
The statistics speak clearly: trauma patients transported by helicopter are 57.0% less likely to die than those transported by ground ambulance, and patient outcomes are improved with use of trauma systems that rely on air transport. These improvements translate to better patient outcomes, reduced healthcare costs, and enhanced quality of life for those requiring specialized medical care.
As Boston-area hospitals face increasing demands for specialized services and serve patients from ever-wider geographic areas, the role of expert medical air transport coordination will only grow in importance. ParaFlight's success demonstrates how specialized aviation concierge services can bridge geographical barriers and time constraints that challenge traditional healthcare delivery models.
For Boston-area hospitals, patients, and families facing medical emergencies, ParaFlight represents more than just transportation coordination—it represents expertise, safety, and the unwavering commitment to preserving life when every second counts. Through its network of certified operators and expert coordination services, ParaFlight ensures that critical medical care is always within reach, regardless of location or circumstances.
The future of medical air transport lies not just in advanced aircraft and medical equipment, but in the expert coordination and industry knowledge that ensures these resources are deployed effectively when lives hang in the balance. ParaFlight's concierge model represents the evolution of medical aviation services, where expertise and safety combine to deliver outcomes that truly matter.
References
- Association of Air Medical Services. "Transport Statistics and Medical Transport Programs." Air Medical Journal. https://www.airmedicaljournal.com/article/S1067-991X(18)30363-8/abstract
- Wikipedia Contributors. "Air Medical Services." Wikipedia. https://en.wikipedia.org/wiki/Air_medical_services
- Center for Health Information and Analysis. "Emergency Department Database (EDD) Reporting." Massachusetts Government. https://www.chiamass.gov/emergency-department-database-edd-reporting/
- Boston Children's Hospital. "Emergency Medicine Department." Boston Children's Hospital. https://www.childrenshospital.org/departments/emergency-medicine
- Federal Aviation Administration. "14 CFR Part 135 Air Carrier and Operator Certification." FAA. https://www.faa.gov/licenses_certificates/airline_certification/135_certification

Introducing Air Nurses x ParaFlight: In-Flight Medical Care, Redefined
Expert Care, In Flight
At ParaFlight, we are proud to offer an exclusive service that goes beyond traditional private jet charters by partnering with Air Nurses, a concierge flight nursing service designed specifically for luxury medical transport in private aviation. Together, we provide a seamless and elevated in-flight medical experience, ensuring that comfort and medical expertise go hand-in-hand throughout the entire journey.
.png)
Who Is Air Nurses?
Air Nurses is a luxury concierge medical service offering board-certified flight nurses who provide comprehensive in-flight medical care. Founded by Ericka Essington BSN, RN, NRP, CFRN, FP-C, CMTE with over 15 years of experience in critical care transport and aviation medicine. Air Nurses have set the bar for medical oversight in private aviation. With Air Nurses, you have a team of elite, aviation-experienced professionals who are solely dedicated to providing medical care and peace of mind during the flight. They come on board your flight as additional crew, seamlessly integrating with your team to ensure continuous medical oversight throughout the journey.
Whether assisting with post-surgical recovery, managing chronic conditions, supporting elderly and pediatric travelers, or offering care for individuals with cognitive needs or those requiring additional support during recovery and wellness transitions, Air Nurses delivers a calm, capable presence onboard, ensuring seamless continuity and comfort from the moment you leave the ground to your final destination.
How Air Nurses Elevates ParaFlight’s Services
• In-Flight Medical Expertise: Air Nurses provide expert medical care aboard private jets, ensuring clients receive real-time monitoring, medication management, and mobility assistance, all while maintaining the highest standard of care. This clinical oversight guarantees that clients with complex medical needs travel safely and comfortably.
• Tailored Medical Solutions: Air Nurses offer customized solutions for each individual flight. From personalized medications and medical equipment to specific care protocols, Air Nurses ensure that every need is anticipated and addressed before departure, allowing clients to travel with confidence.
• Door-to-Destination Care: Air Nurses provide seamless, door-to-destination care, from bedside-to-aircraft transfers to arrival at the destination, ensuring continuous care throughout the entire journey.
• Coordinated Care: Air Nurses work in tandem with ParaFlight and any relevant physicians, family offices, and destination teams, making sure the journey is as smooth and efficient as possible. This seamless coordination enhances the overall experience, ensuring that all aspects of the trip, medical and logistical.are perfectly aligned.
• Luxury and Precision: By adding Air Nurses to ParaFlight’s suite of services, we deliver not only luxury aviation but also peace of mind for travelers with medical needs. This seamless integration of luxury aviation and medical care provides clients with a solution that meets both their comfort and health needs.
A New Class of Medically Supported Travel
Air Nurses and ParaFlight are elevating the standard for in-flight medical care, offering a refined alternative built specifically for private aviation. Every mission combines clinical expertise with seamless charter execution, delivering calm, comfort, and continuity at altitude.
Let’s Build the Mission Around You
For tailored itineraries and onboard medical support, contact our team 24/7:
📧 info@paraflight.aero
📞 1-844-538-1911 (Immediate Assistance)