.png)
Introducing Air Nurses x ParaFlight: In-Flight Medical Care, Redefined
Expert Care, In Flight
At ParaFlight, we are proud to offer an exclusive service that goes beyond traditional private jet charters by partnering with Air Nurses, a concierge flight nursing service designed specifically for luxury medical transport in private aviation. Together, we provide a seamless and elevated in-flight medical experience, ensuring that comfort and medical expertise go hand-in-hand throughout the entire journey.
.png)
Who Is Air Nurses?
Air Nurses is a luxury concierge medical service offering board-certified flight nurses who provide comprehensive in-flight medical care. Founded by Ericka Essington BSN, RN, NRP, CFRN, FP-C, CMTE with over 15 years of experience in critical care transport and aviation medicine. Air Nurses have set the bar for medical oversight in private aviation. With Air Nurses, you have a team of elite, aviation-experienced professionals who are solely dedicated to providing medical care and peace of mind during the flight. They come on board your flight as additional crew, seamlessly integrating with your team to ensure continuous medical oversight throughout the journey.
Whether assisting with post-surgical recovery, managing chronic conditions, supporting elderly and pediatric travelers, or offering care for individuals with cognitive needs or those requiring additional support during recovery and wellness transitions, Air Nurses delivers a calm, capable presence onboard, ensuring seamless continuity and comfort from the moment you leave the ground to your final destination.
How Air Nurses Elevates ParaFlight’s Services
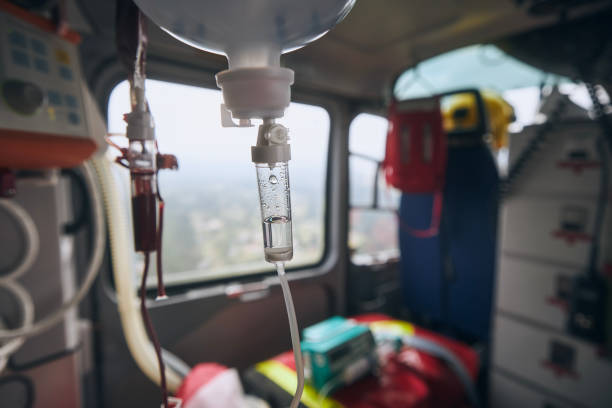
• In-Flight Medical Expertise: Air Nurses provide expert medical care aboard private jets, ensuring clients receive real-time monitoring, medication management, and mobility assistance, all while maintaining the highest standard of care. This clinical oversight guarantees that clients with complex medical needs travel safely and comfortably.
• Tailored Medical Solutions: Air Nurses offer customized solutions for each individual flight. From personalized medications and medical equipment to specific care protocols, Air Nurses ensure that every need is anticipated and addressed before departure, allowing clients to travel with confidence.
• Door-to-Destination Care: Air Nurses provide seamless, door-to-destination care, from bedside-to-aircraft transfers to arrival at the destination, ensuring continuous care throughout the entire journey.
• Coordinated Care: Air Nurses work in tandem with ParaFlight and any relevant physicians, family offices, and destination teams, making sure the journey is as smooth and efficient as possible. This seamless coordination enhances the overall experience, ensuring that all aspects of the trip, medical and logistical.are perfectly aligned.
• Luxury and Precision: By adding Air Nurses to ParaFlight’s suite of services, we deliver not only luxury aviation but also peace of mind for travelers with medical needs. This seamless integration of luxury aviation and medical care provides clients with a solution that meets both their comfort and health needs.
A New Class of Medically Supported Travel
Air Nurses and ParaFlight are elevating the standard for in-flight medical care, offering a refined alternative built specifically for private aviation. Every mission combines clinical expertise with seamless charter execution, delivering calm, comfort, and continuity at altitude.
Let’s Build the Mission Around You
For tailored itineraries and onboard medical support, contact our team 24/7:
📧 info@paraflight.aero
📞 1-844-538-1911 (Immediate Assistance)
Explore All Resources
Browse our full archive of travel guides, educational content, case studies, and service breakdowns.

Private Jet Services for Government Officials in Dallas: Your Complete Guide to Executive Air Travel Solutions
When government operations demand the highest levels of security, efficiency, and flexibility, Dallas-area officials increasingly rely on private aviation services to meet their complex travel requirements. The Dallas-Fort Worth metroplex, serving over 7.6 million residents and functioning as a critical hub for state and federal operations, requires sophisticated transportation solutions that match the gravity of official duties.
As a specialized concierge service, ParaFlight connects government entities with exclusively FAA-certified operators who meet rigorous safety standards and regulatory compliance requirements. We do not directly manage flights, employ crews, or own aircraft, but rather serve as your expert liaison to ensure seamless coordination with the most qualified private aviation providers in the region.
Why Dallas Government Officials Choose Private Aviation
The Dallas-Fort Worth International Airport ranks as the third-busiest airport in the world by aircraft movements and the second-busiest airport in the world by passenger traffic, reflecting the region's critical importance for government operations. From hosting international delegations at major venues to coordinating between numerous federal facilities, officials require transportation solutions that commercial airlines simply cannot accommodate.
Business aviation contributes $150 billion to U.S. economic output and employs more than 1.2 million people, according to the National Business Aviation Association (NBAA). This robust infrastructure directly benefits government operations through enhanced availability and specialized services.
Security and Privacy Advantages
Government officials face unique security challenges that make commercial air travel increasingly complex. Private aviation services through FAA-certified operators offer several critical advantages:
Enhanced Security Protocols: Federal agencies must follow detailed regulatory policy under 41 CFR 102-33 for aircraft management and operations. Private aviation companies specializing in government contracts maintain security standards that include background-checked crew members, secure ground handling, and controlled aircraft access.
Confidential Communications: Private jets provide secure environments for sensitive conversations and document review during flight. With proper security configurations, officials can conduct business without concern for information security.
Operational Flexibility: Unlike commercial flights with fixed schedules, private jets can accommodate last-minute changes, emergency situations, and multi-city itineraries essential for government operations.
Dallas Private Aviation Infrastructure
The Dallas-Fort Worth region features one of the nation's most comprehensive private aviation infrastructures. Dallas–Fort Worth is one of the world's busiest airports when looking at aircraft movements, with a significant portion of these flights accounted for by private aviation.
Key Airports Serving Government Aviation
Dallas Love Field (DAL): Located minutes from downtown Dallas, Love Field offers dedicated private aircraft terminals with streamlined procedures. Located in downtown Dallas, Dallas Love Field offers high-end FBO services through operators like Signature Flight Support and Atlantic Aviation, with well-regarded general aviation facilities.
Dallas Executive Airport (RBD): Located 25 minutes from Dallas–Fort Worth, Dallas Executive Airport is ideal for bypassing busier airspace, with FBOs such as Ambassador Jet Center and Jet Center of Dallas offering services for private travelers.
Addison Airport (ADS): One of the busiest general aviation airports nationally, Addison handles extensive private aircraft operations with sophisticated fixed-base operators (FBOs) providing specialized government and executive travel services.
Dallas-Fort Worth International Airport (DFW): The airport has a General Aviation Terminal with facilities and services available to private flight passengers, and supports private jets.
Professional Ground Services
Private jet services in Dallas extend beyond aircraft operations. Government officials benefit from:
- Expedited Security Screening: Procedures specifically designed for private aviation that maintain security standards while reducing processing time
- Ground Transportation Coordination: Integration with secure ground transportation when required
- Concierge Services: Full-service support including catering, communications setup, and meeting facilities at FBO locations
Aircraft Options for Government Operations
The diversity of FAA-certified aircraft available through our network ensures government officials can select appropriate options for specific mission requirements.
Light Jets for Regional Operations
For travel within Texas or to neighboring states, light jets offer efficient solutions while maintaining necessary speed and convenience for government operations. These aircraft typically accommodate 6-8 passengers and are suitable for small delegations or individual travel with security details.
Mid-Size Jets for National Travel
When government business requires travel to other major metropolitan areas, mid-size jets provide the range and comfort necessary for productive flight time. These aircraft can reach most destinations within the continental United States without refueling stops.
Heavy Jets for International Missions
For international travel or cross-country trips requiring maximum comfort and range, heavy jets offer spacious cabins, extended range capabilities, and amenities necessary for long-distance government operations.
Specialized Government Aircraft
Some FAA-certified operators maintain aircraft specifically configured for government use, featuring:
- Enhanced Communication Systems: Satellite communications, secure internet connectivity, and encrypted voice communications
- Modified Cabin Layouts: Conference areas, secure document storage, and specialized seating arrangements
- Security Equipment: Advanced systems and protective measures appropriate for government operations
Cost Considerations and Budget Planning
While private jet travel represents a significant expense, government entities must evaluate costs against the value of time saved, enhanced security, and operational flexibility. Industry estimates suggest private jet hourly operating costs in the Dallas market range from approximately $2,500 for light jets to over $8,000 for heavy jets, not including positioning fees and ancillary costs.
Cost-Benefit Analysis Framework
Effective government entities conduct thorough analyses considering:
Time Value: When calculated against the hourly compensation of senior government officials and their staffs, private jet travel may prove more economical than time lost to commercial airline delays and connections.
Productivity Enhancement: The ability to conduct secure meetings and review sensitive materials during flight can transform travel time from lost productivity into valuable working hours.
Security Considerations: The enhanced security provided by private aviation may eliminate the need for additional security measures required for commercial travel.
Strategic Budget Planning
Successful government use of private aviation requires careful budget planning:
- Annual Service Agreements: Many operators offer preferred rates for guaranteed annual flight commitments
- Collaborative Services: Regional cooperation between government entities can reduce per-flight costs through shared aircraft utilization
- Emergency Preparedness: Maintaining dedicated budgets for urgent travel situations ensures availability when needed
Regulatory Compliance and Oversight
Government use of private aviation operates under strict regulatory oversight to ensure appropriate use of public resources and maintain transparency.
Federal Requirements
GSA publishes regulatory policy (41 CFR 102-33.215 and 41 CFR 102-33.220) to clarify the terms of "public" use of Government aircraft. The General Services Administration provides comprehensive guidelines including:
- Approval Requirements: Multi-level authorization processes for private aircraft use
- Documentation Standards: Detailed record-keeping requirements for all government flights
- Cost Justification: Mandatory analysis demonstrating private aircraft use efficiency compared to commercial alternatives
State and Local Oversight
Texas state agencies and local governments operate under additional requirements:
- Public Records Compliance: Flight records, costs, and justifications subject to public information requests
- Ethics Guidelines: Strict guidelines preventing personal use of government-funded aviation services
- Procurement Standards: Competitive processes for aviation service contracts
Selecting Qualified Service Providers
Government entities must carefully evaluate private aviation providers to ensure they meet public sector operational requirements.
Critical Selection Criteria
Safety Standards: Business aircraft have a safety record that is comparable to that of the major airlines. Operators must maintain exemplary safety records with current certifications and clean inspection histories.
Regulatory Compliance: Crew members and ground personnel should hold appropriate clearances when handling sensitive government operations.
Insurance Coverage: Comprehensive liability coverage appropriate for government operations, typically exceeding $100 million in coverage limits.
Operational Availability: 24/7 availability for emergency situations and last-minute schedule changes.
Comprehensive Vetting Process
Thorough evaluation should include:
- Financial Stability Assessment: Evaluation of operator financial condition to ensure reliable service delivery
- Reference Verification: Contact with other government clients to verify service quality and reliability
- Facility Inspections: On-site evaluation of maintenance facilities, security procedures, and operational capabilities
- Pilot Qualifications: Review of pilot experience, training records, and ongoing proficiency requirements
Technology Integration and Communication Systems
Modern government operations require sophisticated technology integration during air travel. Leading FAA-certified operators in Dallas can provide:
Current Connectivity Solutions
High-Speed Internet: Satellite-based internet connectivity enabling real-time communication and document sharing during flight.
Secure Communication Systems: Encrypted voice and data communications meeting applicable government security standards.
Video Conferencing: Equipment and connectivity supporting secure video conferences from aircraft cabins.
Mobile Office Configuration
Private jets can be configured as mobile offices, featuring:
- Work Surfaces: Tables and desk areas suitable for document review and computer work
- Power Systems: Multiple power outlets and USB charging ports for electronic devices
- Storage Solutions: Secure storage for sensitive documents and equipment
- Lighting Systems: Adjustable lighting optimized for reading and computer work
Environmental Considerations and Sustainability
As government entities face increasing pressure to address environmental concerns, private aviation providers are developing more sustainable operational practices.
Current Efficiency Improvements
Modern private jets incorporate technologies that improve fuel efficiency:
- Advanced Engines: New engine designs that reduce fuel consumption
- Aerodynamic Enhancements: Winglets and other improvements that reduce drag and fuel burn
- Weight Reduction: Advanced materials and design techniques that reduce aircraft weight
Carbon Offset Programs
Many private aviation operators now offer carbon offset programs, allowing government entities to address the environmental impact of their air travel through verified offset projects.
Sustainable Aviation Fuel (SAF)
The increasing availability of sustainable aviation fuel provides government entities with options to reduce environmental impact. SAF can reduce lifecycle carbon emissions compared to conventional jet fuel, though availability and cost considerations vary by location.
Future Trends in Government Private Aviation
The private aviation industry continues to evolve, with several trends particularly relevant to government operations:
Emerging Technologies
Electric and Hybrid Aircraft: Companies are developing electric aircraft for short-distance travel, potentially suitable for regional government operations within Texas in the future.
Enhanced Security Technology: Advanced security technologies, including biometric identification systems and threat assessment capabilities, may be integrated into private aircraft operations to meet evolving government security requirements.
Artificial Intelligence Applications: Future AI-powered systems may optimize flight planning, predict maintenance requirements, and enhance operational efficiency in ways that could benefit government operations.
Best Practices for Government Private Aviation Programs
Successful government private aviation programs demonstrate several key characteristics:
Comprehensive Policies and Procedures
- Clear Usage Guidelines: Detailed policies outlining appropriate circumstances for private aircraft use
- Approval Workflows: Streamlined but thorough approval processes balancing efficiency with oversight
- Cost Tracking Systems: Systems for tracking and reporting all aviation-related expenses
Regular Program Evaluation
- Performance Metrics: Key performance indicators measuring program effectiveness and efficiency
- Cost Analysis: Regular comparison of private aviation costs against commercial alternatives
- Stakeholder Feedback: Systematic collection of feedback from users to identify improvement opportunities
Transparency and Accountability
- Public Reporting: Regular public reports on private aviation usage and costs
- Audit Compliance: Cooperation with internal and external audits of aviation programs
- Media Relations: Proactive communication about the business case for private aviation use
How ParaFlight Facilitates Government Aviation Solutions
As your specialized aviation concierge service, ParaFlight streamlines the complex process of coordinating government private aviation. Our expert-driven approach includes:
Operator Verification: We maintain relationships exclusively with FAA-certified operators who meet rigorous safety and compliance standards.
Regulatory Compliance Support: Our team understands government aviation requirements and ensures all arrangements comply with applicable regulations.
Cost Optimization: We leverage our industry relationships to secure competitive pricing while maintaining service quality standards.
24/7 Coordination: Our experienced team provides round-the-clock support for urgent government travel requirements.
Documentation Assistance: We help ensure proper documentation and record-keeping to meet government reporting requirements.
Conclusion
Private jet services for government officials in Dallas represent a critical component of efficient, secure government operations. With the region's sophisticated aviation infrastructure, diverse aircraft options, and experienced FAA-certified service providers, government entities can access professional private aviation services that meet their unique operational requirements.
The key to successful government private aviation programs lies in careful planning, rigorous oversight, and transparent operations that demonstrate appropriate stewardship of public resources. As the private aviation industry continues to evolve with new technologies and enhanced capabilities, government entities in Dallas are well-positioned to benefit from these advances while maintaining the highest standards of security, efficiency, and accountability.
By partnering with ParaFlight's expert concierge services, Dallas-area government entities can ensure their officials have access to reliable, secure, and efficient transportation necessary to serve the public effectively in an increasingly complex and fast-paced environment.
References
- General Services Administration. (2024). Aviation regulations and guidance. https://www.gsa.gov/policy-regulations/policy/aviation-management-policy/aviation-regulations-and-guidance
- National Business Aviation Association. (2024). Business Aviation: Just the Facts. https://nbaa.org/business-aviation/business-aviation-just-the-facts/
- Federal Aviation Administration. (2024). General Aviation and Part 135 Activity Surveys. https://www.faa.gov/data_research/aviation_data_statistics/general_aviation
- Dallas Fort Worth International Airport. (2024). Traffic Statistics. https://www.dfwairport.com/business/about/stats/
- Bureau of Transportation Statistics. (2024). Air Travel Consumer Report: October 2024 Numbers. https://www.bts.gov/newsroom/air-travel-consumer-report-october-2024-numbers

Fastest MEDEVAC Flight Coordination in Phoenix: How Expert Planning Saves Lives Through Rapid Response Aviation
When medical emergencies strike in the Phoenix metropolitan area, every second counts toward connecting patients with life-saving care. Medical evacuation (MEDEVAC) services represent the critical bridge between emergency scenes and specialized medical facilities, requiring precise coordination with FAA-certified operators who conduct helicopter air ambulance operations under strict Part 135 requirements. Phoenix, Arizona's fifth-largest city with over 1.7 million residents, relies on sophisticated flight coordination expertise to ensure the fastest possible emergency medical response times across the sprawling Sonoran Desert landscape.
At ParaFlight, we specialize in coordinating these critical medical transportation services by connecting families and medical facilities with qualified, FAA-certified air medical operators throughout the Phoenix region. Our expert-driven approach ensures seamless coordination when minutes matter most.
Understanding MEDEVAC Flight Coordination Excellence in Phoenix
Medical evacuation flight coordination involves orchestrating a complex network of emergency medical services, FAA Part 135 certified aviation operators, hospital systems, and communication centers working in perfect synchronization. In Phoenix, this intricate coordination system serves not only the metropolitan area but extends across rural Arizona, where ground transportation to major medical facilities can take hours.
The Phoenix MEDEVAC system operates under strict Federal Aviation Administration (FAA) guidelines, with aircraft using the "MEDEVAC" designation to receive priority handling from air traffic controllers. This coordination extends to Phoenix Sky Harbor International Airport, one of the busiest airports in the United States handling over 44 million passengers annually.
The Critical Timeline: Understanding Emergency Response
The first 60 minutes after traumatic injury has been termed the "golden hour," a concept that has been taught and practiced for more than 3 decades. However, recent scientific evidence suggests the "golden hour" concept is pervasive despite little evidence to support it. Research indicates that median emergency response times from 911 call to hospital arrival average 36.3 minutes across diverse North American locations.
In Phoenix's urban sprawl covering over 500 square miles, ground ambulances face significant challenges including traffic congestion, distance to trauma centers, and harsh desert conditions. Medical evacuation operations provide rapid response capabilities, with helicopters offering agility for urban areas and rugged terrain access.
Phoenix's MEDEVAC Infrastructure and Certified Operators
Working with FAA-Certified MEDEVAC Providers
Phoenix benefits from multiple FAA-certified MEDEVAC operators, each maintaining strategically positioned aircraft throughout the metropolitan area. ParaFlight coordinates with these certified operators to ensure optimal coverage and response capabilities.
These certified operators maintain aircraft equipped with advanced life support equipment and staffed by experienced flight nurses and paramedics who meet stringent certification requirements including nationally registered EMT-P status, extensive critical care experience, and current ACLS, ITLS, CPR, and PALS certifications.
State-of-the-Art Medical Aircraft Standards
Modern MEDEVAC helicopters are specialized aircraft equipped with medical equipment and personnel to swiftly transport patients to hospitals or trauma centers. These FAA-certified aircraft feature:
- Advanced cardiac monitoring systems
- Ventilators and airway management tools
- Blood and medication storage capabilities
- Satellite communication systems for real-time medical consultation
- Night vision capabilities for 24/7 operations
- GPS navigation systems with hospital landing zone databases
The Phoenix Advantage: Geographic and Operational Benefits
Optimal Flying Conditions for Emergency Operations
Phoenix's desert climate provides significant advantages for MEDEVAC operations. With over 300 sunny days annually and minimal precipitation, weather-related flight restrictions are less common compared to other major metropolitan areas. FAA regulations require certified operators to obtain weather reports from approved sources within 15 nautical miles of airports for safe operations.
Strategic Hospital Network Integration
Phoenix's trauma care system includes several Level I trauma centers equipped with helipads designed for rapid patient transfer. The city's medical infrastructure supports seamless integration between air and ground emergency services through coordinated planning.
Advanced Communication and Expert Coordination Systems
Unified Emergency Response Through Expert Planning
Phoenix's MEDEVAC coordination relies on sophisticated communication systems connecting multiple agencies through expert coordination services like ParaFlight:
911 Emergency Dispatch Centers immediately assess situations requiring air medical transport, considering factors such as injury severity, location accessibility, and hospital capacity.
Flight Operations Centers coordinate with FAA-certified operators for aircraft deployment, weather monitoring, and air traffic control communications to ensure optimal flight paths and minimal response times.
Hospital Communication Networks provide real-time updates on trauma bay availability, specialist coverage, and landing zone conditions.
Technology Integration in Coordination Services
Modern MEDEVAC coordination utilizes advanced technology including:
- Automated vehicle location (AVL) systems tracking emergency response assets
- Computer-aided dispatch (CAD) systems providing instant access to medical facility capabilities
- Weather monitoring systems providing real-time atmospheric conditions
- GPS-based navigation with obstacle databases for safe low-altitude flight operations
Response Time Performance and Industry Standards
According to the Association of Air Medical Services (AAMS), established in 1980, the organization is dedicated to advancing transport medicine through advocacy, education, and research to ensure high-quality, life-saving care. Industry benchmarks suggest optimal response targets, though actual performance varies by location and circumstances.
Estimated optimal MEDEVAC response goals include:
- Dispatch to airborne: Under 8 minutes (industry estimate)
- Scene response time: 15-20 minutes for urban areas (estimated)
- Patient transport time: Minimized through strategic hospital selection
- Total response time: Under 30 minutes for most metropolitan emergencies (estimated)
Note: These are industry estimates and actual response times may vary based on numerous factors including weather, aircraft availability, and specific circumstances.
Challenges and Solutions in Desert MEDEVAC Operations
Environmental Considerations for Certified Operators
Operating MEDEVAC services in Phoenix's Sonoran Desert environment presents unique challenges for FAA-certified operators:
Temperature Extremes: Summer temperatures exceeding 120°F affect aircraft performance and require specialized procedures. FAA regulations require pilots to demonstrate familiarity with local flying areas through examination within 12 months.
Dust and Visibility: Desert dust storms (haboobs) can rapidly reduce visibility, requiring sophisticated weather monitoring and alternative transport protocols.
Terrain Obstacles: Phoenix's mountainous terrain requires specialized navigation capabilities and obstacle avoidance systems for safe operations.
Urban Aviation Coordination Challenges
Phoenix's rapid urban development creates ongoing coordination challenges:
Infrastructure Complexity: Extensive electrical infrastructure requires detailed mapping and specialized navigation for safe low-altitude operations.
Traffic Considerations: While helicopters avoid ground traffic, landing zone access coordination can be complicated by traffic patterns.
Community Integration: Balancing rapid response requirements with community considerations requires careful flight path planning.
Training and Certification Excellence Standards
Medical Crew Certification Requirements
Phoenix MEDEVAC operations maintain strict medical staffing standards, with flight nurses requiring critical care experience and advanced certifications, while flight paramedics need extensive advanced life support experience and specialized equipment training.
Transport nursing represents a unique and expanded role encompassing air and surface medical transport of critically ill and injured patients.
Pilot Certification Standards
MEDEVAC pilots must meet stringent FAA requirements including commercial or airline transport pilot licenses with instrument ratings, with dispatcher certifications preferred. Additional requirements typically include:
- Minimum flight hours with significant helicopter experience
- Instrument flight rating with night vision qualifications
- Mountain flying experience and desert operation familiarity
- Regular recurrent training in emergency procedures
Integration with Regional Emergency Systems Through Expert Coordination
Multi-State Coordination Capabilities
Phoenix's MEDEVAC system frequently requires coordination with neighboring states for specialized care transfers. Patients requiring treatment unavailable in Phoenix may need transport to facilities in California, Colorado, or Utah, requiring complex inter-state medical transport coordination expertise.
Rural Arizona Coverage Extension
Phoenix-based coordination services extend coverage throughout rural Arizona, where ground transport distances to trauma centers can exceed 200 miles. This coordination requires:
- Extended range capability planning
- Communication with remote landing zones
- Coordination with volunteer emergency services
- Weather monitoring across diverse geographic regions
Quality Assurance and Continuous Improvement
Performance Monitoring Systems
AAMS advocates on behalf of the medical transport community to ensure sustainability, increase medical quality and patient safety. Quality assurance programs include:
Response Time Analysis: Continuous monitoring of coordination efficiency and transport effectiveness.
Safety Management Systems: Comprehensive safety programs tracking incidents and implementing preventive measures.
Outcome Assessment: Following coordination effectiveness to improve future response planning.
Future Innovation in Coordination Technology
Phoenix MEDEVAC coordination services are preparing for emerging technologies:
Enhanced Communication Networks: Future 5G-enabled capabilities may provide improved connectivity between coordination centers and medical facilities.
Predictive Analytics: Data-driven systems for demand pattern prediction and optimal resource positioning are being developed.
Autonomous Systems Integration: Future autonomous flight systems may enhance safety and operational efficiency, though these remain in development phases.
Economic Impact and Community Benefits
Healthcare System Integration Benefits
Expert MEDEVAC coordination provides significant benefits to Phoenix's healthcare system:
- Improved emergency department efficiency through strategic patient distribution
- Enhanced trauma center utilization optimization
- Reduced coordination complexity for hospital staff
- Streamlined communication between multiple providers
Community Safety Enhancement
Professional MEDEVAC coordination services enhance overall community safety by ensuring rapid access to qualified, FAA-certified operators when emergencies occur. This coordination infrastructure supports Phoenix's continued growth and development.
Future Developments in Phoenix MEDEVAC Coordination
Emerging Technologies on the Horizon
Phoenix MEDEVAC coordination is monitoring technological advances for future integration:
Electric Aircraft Development: Research into electric MEDEVAC helicopters may offer reduced operating costs and environmental impact in the future.
Unmanned Systems Research: Development of drone technology for medical supply delivery and scene assessment remains in experimental phases.
AI-Enhanced Coordination: Artificial intelligence applications for coordination optimization are being researched, though not yet operationally deployed.
Expansion and Growth Planning
As Phoenix continues rapid population growth, coordination services are expanding:
- Enhanced coordination capabilities with additional certified operators
- Improved integration with emerging hospital systems
- Expanded coverage areas serving Arizona's growing population
- Advanced training and coordination capabilities
The ParaFlight Advantage: Expert-Driven MEDEVAC Coordination
Why Choose Professional Coordination Services
ParaFlight's expert-driven coordination model provides several key advantages:
Exclusive Partnership with FAA-Certified Operators: We work only with fully certified, compliant operators who meet the highest safety and operational standards.
24/7 Expert Coordination: Our experienced team provides round-the-clock coordination services, ensuring rapid response when emergencies occur.
Comprehensive Network Access: Through our established relationships with certified operators, we can coordinate the most appropriate aircraft and crew for each specific situation.
Regulatory Compliance Assurance: Our expertise ensures all coordinated flights meet FAA requirements and industry safety standards.
Our Coordination Process
When you contact ParaFlight for MEDEVAC coordination in Phoenix:
- Immediate Assessment: Our experts rapidly assess your specific medical transportation needs
- Operator Selection: We coordinate with the most appropriate FAA-certified operator for your situation
- Comprehensive Planning: We handle all coordination details including hospital communication, flight planning, and regulatory compliance
- Ongoing Support: We provide continuous coordination support throughout the entire transport process
Conclusion: Excellence in MEDEVAC Coordination When Lives Depend on It
Phoenix's MEDEVAC coordination success depends on expert planning, qualified operators, and sophisticated coordination systems working together seamlessly. By leveraging aviation assets and specialized medical expertise, these services facilitate timely access to critical care and enhance outcomes for patients in need through seamless coordination between healthcare providers, aviation professionals, and emergency responders.
ParaFlight's commitment to coordinating exclusively with FAA-certified operators ensures Phoenix residents and visitors receive optimal emergency medical transportation coordination when every second counts. Our expert-driven approach provides the professional coordination needed to navigate complex emergency medical transportation requirements while maintaining the highest safety and compliance standards.
Through ongoing relationship building with certified operators, continuous training, and system optimization, ParaFlight's coordination services continue setting standards for emergency medical aviation coordination nationwide, providing essential support for over two million metropolitan area residents and countless visitors to the Valley of the Sun.
When medical emergencies require immediate air transport coordination in Phoenix, trust ParaFlight's expertise to connect you with qualified, FAA-certified operators who can provide the life-saving transportation services you need.
References
- Federal Aviation Administration - Part 135 Helicopter Air Ambulance Operations
- Emergency Medical Services Intervals and Survival in Trauma - National Center for Biotechnology Information
- Association of Air Medical Services - Industry Leadership
- Federal Aviation Administration - MEDEVAC Flight Priority
- The Journalist's Resource - Emergency Medical Services Response Times
Booking a Medical Jet Charter in Philadelphia: Your Complete Guide with ParaFlight
When medical emergencies arise or specialized treatment requires travel, time becomes the most critical factor. For residents of Philadelphia and the surrounding areas, medical jet charter services provide life-saving transportation that bridges the gap between urgent medical needs and quality healthcare facilities. ParaFlight serves as your expert concierge partner, connecting you with FAA-certified operators who deliver hope, comfort, and critical care when every second counts.
Why Choose Medical Jet Charter Services?
Medical jet charter services have revolutionized emergency medical transportation and planned medical travel. Unlike commercial airlines, which have numerous restrictions and delays, medical jets are specifically equipped and staffed to handle patients requiring specialized care during transport.
The advantages of medical jet charter include immediate availability, specialized medical equipment, qualified medical personnel onboard, and the ability to fly directly to the nearest appropriate medical facility. Approximately 3% of all ambulance transports in the United States are performed by aeromedical assets, requiring over 300 air ambulance services, 1000 bases, and 1400 registered aircraft, according to the National Center for Biotechnology Information.
Philadelphia: A Strategic Location for Medical Air Transport
Philadelphia's position on the East Coast makes it an ideal hub for medical jet charter services. The city is home to some of the nation's most prestigious medical institutions, including the Hospital of the University of Pennsylvania, Jefferson Health, and Children's Hospital of Philadelphia (CHOP). However, patients often need transport to specialized facilities in other cities like Boston, New York, or even international destinations.
The Philadelphia region is served by multiple airports capable of handling medical jet operations, including Philadelphia International Airport (PHL), Northeast Philadelphia Airport (PNE), and Wings Field Airport (LOM). This network ensures that ParaFlight's partner operators can coordinate efficient medical flights regardless of weather conditions or air traffic constraints.
Types of Medical Jet Charter Services
Emergency Medical Transport
Emergency medical jet charter services are designed for critical situations where patients require immediate transport to specialized medical facilities. These flights operate 24/7 and can typically be airborne within 30-60 minutes of receiving a call. Aircraft operated by Part 135 certificate holders authorized by the Administrator to conduct helicopter air ambulance operations are equipped with advanced life support systems, ventilators, cardiac monitors, and other critical care equipment.
Emergency medical jets are staffed with certified flight nurses, paramedics, and when necessary, specialized physicians. Helicopters are ideal for transporting critical trauma patients because they are more effective in decreasing the time of transport to a trauma hospital. This is important because, for many critical trauma patients, the most important factor in decreasing mortality is getting them quickly to an operating room with a trauma surgeon.
Planned Medical Transport
Not all medical jet charter needs are emergencies. Planned medical transport serves patients who require specialized treatment at distant facilities but are stable enough for scheduled transport. This might include patients seeking treatment at renowned cancer centers, transplant facilities, or specialized pediatric hospitals.
Planned medical flights offer more flexibility in terms of timing and can often accommodate family members or caregivers. These flights are typically more cost-effective than emergency transports and allow for better coordination with receiving medical facilities.
Organ Transport
Philadelphia's medical institutions frequently participate in organ transplant programs, making rapid organ transport crucial. Medical jets equipped for organ transport maintain precise temperature and environmental controls necessary to preserve organs during transport. Time is especially critical in organ transport, as organs have limited viability outside the body.
International Medical Repatriation
For Philadelphia residents who become ill or injured while traveling abroad, international medical repatriation services provide transport back to familiar healthcare systems. These flights often require additional documentation, customs clearance, and coordination with international authorities.
ParaFlight: Your Expert Concierge Partner
ParaFlight distinguishes itself in the medical jet charter industry by serving as your dedicated concierge partner, connecting you exclusively with FAA-certified operators who maintain the highest standards of safety and medical care. Rather than owning aircraft or employing medical crews directly, ParaFlight leverages its extensive network of certified providers to ensure you receive the most appropriate and qualified medical transport services for your specific needs.
Our Partner Network
ParaFlight works exclusively with Part 135 certificate holders who maintain FAA certifications and medical personnel certified in advanced life support, flight medicine, and critical care transport. Our partner network includes operators whose teams comprise registered nurses with flight experience, paramedics trained in air medical protocols, and on-call physicians for complex cases. Each partner operator's crew members undergo continuous education and recertification to maintain the highest standards of medical care.
Fleet and Equipment Standards
Our partner operators maintain medical jets equipped with hospital-grade medical equipment including ventilators, defibrillators, IV pumps, cardiac monitors, and specialized equipment for pediatric and neonatal transport. Each aircraft maintains redundant systems to ensure continuous operation of critical medical devices throughout the flight.
The aircraft interiors are designed specifically for medical transport, with easy patient loading systems, adequate space for medical personnel to work, and secure mounting points for all medical equipment. Advanced communication systems allow medical teams to consult with receiving physicians during flight.
The Medical Jet Charter Process with ParaFlight
Initial Consultation
When you contact ParaFlight for medical jet charter services, our expert coordination team immediately begins the process of understanding your specific medical transport needs. This includes assessing the patient's medical condition, determining the urgency of transport, identifying the destination facility, and coordinating with our network of certified operators and medical teams at both origin and destination.
Medical Assessment and Partner Selection
Our team works with qualified medical professionals to review all available medical information and determine the appropriate level of care required during transport. This assessment helps us select the most qualified partner operator, determine staffing requirements, necessary equipment, and any special considerations for the flight.
Flight Planning and Coordination
ParaFlight's coordination team manages all aspects of the transport through our certified operator partners, including airport arrangements, customs and immigration requirements for international flights, ground ambulance coordination, and communication with receiving medical facilities.
Transport Execution
On the day of transport, our partner operator's ground team coordinates with the referring medical facility to ensure smooth patient transfer. The certified medical crew takes responsibility for the patient's care from departure to arrival, providing continuous monitoring and medical intervention as needed.
Cost Considerations and Insurance Coverage
Medical jet charter services represent a significant financial investment, with costs typically ranging from $15,000 to $50,000 for domestic flights within the United States, according to industry estimates. International flights can cost significantly more depending on distance, route complexity, and regulatory requirements.
Many insurance plans, including Medicare and private health insurance, provide coverage for medically necessary air transport when certain criteria are met. According to healthcare industry sources, air ambulance services must be deemed medically necessary and the patient must require services or equipment only available on air ambulances for coverage to apply.
ParaFlight works closely with insurance providers to verify coverage and ensure proper documentation for reimbursement. Our specialists understand the complex requirements for medical transport coverage and can help families navigate the insurance approval process.
Safety Standards and Regulatory Compliance
Safety is paramount in medical aviation. ParaFlight exclusively partners with operators who maintain 14 CFR Part 135 Air Carrier and Operator Certification from the Federal Aviation Administration (FAA), adhere to standards set by the Commission on Accreditation of Medical Transport Systems (CAMTS), a peer review organization dedicated to improving patient care and safety, and follow protocols established by the Association of Air Medical Services.
CAMTS is an independent, non-profit agency based in Sandy Springs, South Carolina, which audits and accredits fixed-wing, rotary wing, and surface medical transport services worldwide to a set of industry-established criteria. Our partner operators undergo rigorous training in medical flight operations, including specialized approaches to hospitals, weather minimums for medical flights, and coordination with air traffic control for priority handling.
Market Growth and Industry Statistics
The medical jet charter industry continues to expand significantly. The global air ambulance services market size was estimated at USD 14.6 billion in 2022 and is expected to grow at a CAGR of 10.7% from 2023 to 2030, according to Grand View Research. This growth reflects increasing recognition of the value these services provide in emergency medical care and planned medical transport.
Annually, critical care transport teams conduct approximately 300,000 rotor wing, 230,000 critical care ground, and 40,000 fixed wing transports, demonstrating the substantial demand for specialized medical transportation services.
Choosing the Right Medical Jet Charter Provider
When selecting a medical jet charter service in Philadelphia, consider several key factors:
Accreditation and Certifications
Look for providers who work exclusively with CAMTS-accredited operators and FAA Part 135 certified aircraft operators. These credentials ensure adherence to the highest safety and medical care standards.
Response Time and Coordination
Emergency medical situations require rapid response and expert coordination. Quality providers should be able to coordinate launches within one hour for emergency calls and provide realistic timeframes for planned transports through their network of certified operators.
Medical Capabilities
Ensure the provider can coordinate access to operators with your specific medical needs, whether that involves specialized equipment, particular medical personnel qualifications, or experience with your type of medical condition.
Insurance Coordination and Expert Guidance
Choose providers experienced in working with insurance companies and familiar with coverage requirements for medical transport. ParaFlight's concierge approach includes dedicated support throughout the insurance verification and approval process.
Future Innovations in Medical Air Transport
The medical aviation industry continues to evolve with advancing technology. Future innovations may include enhanced telemedicine capabilities for real-time consultation between flight crews and ground-based physicians, improved aircraft designs optimized for patient transport, and emerging technologies like autonomous systems that could enhance safety and efficiency in medical aviation operations.
While current operations rely on proven technologies and established protocols, the industry continues to explore how artificial intelligence and other emerging technologies might support improved patient outcomes and operational efficiency in the years ahead.
Conclusion
Medical jet charter services provide critical transportation for patients requiring specialized medical care or emergency transport. In Philadelphia, where world-class medical facilities attract patients from around the globe, medical air transport serves as a vital link between patients and the care they need.
ParaFlight combines expert coordination with access to the industry's most qualified, FAA-certified operators to provide comprehensive medical jet charter services. Our commitment to working exclusively with accredited providers ensures that patients and families receive the highest standards of safety, medical care, and customer service during challenging medical situations.
Whether facing a medical emergency requiring immediate transport or planning travel for specialized treatment, ParaFlight provides the expert concierge services Philadelphia residents can trust. Call ParaFlight today to learn how our medical air transport coordination services can serve your healthcare transportation needs through our network of certified operators.
References
- Loyd JW, Larsen T, Kuhl EA, et al. Aeromedical Transport. StatPearls [Internet]. 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK518986/
- Air Ambulance Services Market Size & Share Report. Grand View Research. 2023. Available from: https://www.grandviewresearch.com/industry-analysis/air-ambulance-services-market
- Federal Aviation Administration. 14 CFR Part 135 Air Carrier and Operator Certification. Available from: https://www.faa.gov/licenses_certificates/airline_certification/135_certification
- Commission on Accreditation of Medical Transport Systems. About CAMTS. Available from: https://www.camts.org/
Establishing Transport Statistics: Results From the Medevac Transport Statistics Survey. Air Medical Journal. 2019. Available from: https://www.airmedicaljournal.com/article/S1067-991X(18)30363-8/abstract

Rapid Medical Evacuation from Remote Areas: ParaFlight in Action
When medical emergencies strike in remote locations, every second counts. The difference between life and death often hinges on how quickly critically injured or ill patients can access definitive medical care. This is where specialized medical evacuation services like ParaFlight become indispensable lifelines, orchestrating rapid transport that bridges the gap between remote emergencies and world-class medical facilities.
The Critical Nature of Remote Medical Emergencies
Remote areas present unique challenges for emergency medical response. Remote islands face difficulties due to a lack of accessibility, manpower, and facilities, stemming from the uneven distribution of medical resources. The delivery of health services to these areas is particularly challenging because of their relatively small populations and inaccessible locations. Similar challenges exist across mountainous regions, offshore locations, rural communities, and areas affected by natural disasters.
The statistics paint a stark picture of the urgency involved. Statistically speaking, there is one case of emergency medical evacuation per every 4,000 travelers, highlighting how common these emergencies can be for those venturing into remote areas. For those who find themselves in need of evacuation, the total cost of medevac varies by location, ranging from $25,000 for transport within North America to ≥$250,000 for more distant and remote locations.
Understanding the Golden Hour Concept
The foundation of emergency medical response rests on a critical principle known as the "golden hour." In emergency medicine, the golden hour is the period of time immediately after a traumatic injury during which there is the highest likelihood that prompt medical and surgical treatment will prevent death. He wrote in an article that "the first hour after injury will largely determine a critically injured person's chances for survival".
However, recent research has evolved this concept. It is well established that the person's chances of survival are greatest if they receive care within a short period of time after a severe injury; however, there is no evidence to suggest that survival rates drop off after 60 minutes. This has led to the development of the "golden period" concept, recognizing that while rapid response remains crucial, many other patients may have more than an hour–a determination based on the extent of the patient's injuries, not a predetermined time that generalizes all trauma patients.
The Scale of Medical Aviation Operations
The medical aviation industry represents a critical component of modern healthcare infrastructure. The Association of Air Medical Services estimates that more than 550,000 patients in the U.S. rely on air medical transport services annually. More broadly, around 640,000 critical care transfers are conducted annually. Annually, critical care transport teams conduct approximately 300,000 rotor wing, 230,000 critical care ground, and 40,000 fixed wing transports.
Approximately 3% of all ambulance transports in the United States are performed by aeromedical assets, requiring over 300 air ambulance services, 1000 bases, and 1400 registered aircraft. This extensive network ensures that even the most remote locations can potentially access life-saving medical transport when coordinated properly.
Response Time Advantages of Air Medical Services
When comparing helicopter emergency medical services (HEMS) to ground transportation, the time advantages become clear in specific scenarios. Research from Norway provides valuable insights: The median flying time was 19 minutes (25%-75% percentiles: 13-28) for helicopter emergency medical services responding to remote locations.
Studies examining the comparative effectiveness reveal that ground ambulance transport provided the shortest 911-hospital arrival interval at distances less than 10 miles from the hospital. At distances greater than 10 miles, simultaneously dispatched air transport was faster. Nonsimultaneous dispatched helicopter transport was faster than ground if greater than 45 miles from the hospital.
ParaFlight's Concierge Approach to Medical Evacuation
ParaFlight distinguishes itself in the medical aviation landscape through its expert-driven, concierge model that prioritizes patient care coordination and safety. Rather than operating aircraft directly, ParaFlight partners exclusively with FAA-certified operators, ensuring that every medical evacuation meets the highest regulatory standards for safety and operational excellence.
Expert Medical Coordination
The ParaFlight model centers on providing specialized medical evacuation expertise that goes far beyond simple transportation logistics. Our experienced medical professionals assess each situation individually, coordinating with:
- Local emergency responders at the scene
- Receiving hospital medical teams
- FAA-certified aviation operators
- Specialized medical equipment providers
- Family members and care coordinators
This comprehensive approach ensures that patients receive appropriate medical care throughout the entire evacuation process, from initial assessment to delivery at the receiving facility.
Safety Through Partnership
By partnering exclusively with FAA-certified operators, ParaFlight eliminates the operational risks associated with directly managing aircraft, crews, and maintenance programs. Our certified partners maintain rigorous safety standards, including:
- Regular aircraft maintenance and inspection programs
- Highly trained medical flight crews
- Advanced life support equipment and capabilities
- Weather monitoring and flight safety protocols
- Comprehensive insurance coverage
Remote Area Evacuation Challenges
Geographic and Environmental Factors
Remote area medical evacuations present unique challenges that require specialized expertise and equipment. Beyond transportation costs, the geographic isolation of remote areas presents challenges in recruiting and retaining healthcare professionals due to unequal access to education and professional support, the necessity of working beyond their usual scope of practice, safety concerns, and adapting to extreme weather conditions.
Weather conditions are an important consideration for air medical transport. Helicopters are susceptible to heavy weather conditions such as strong winds or heavy snowfall. This is why ParaFlight's coordination expertise becomes invaluable – our teams understand how to work with weather patterns, alternative transport modes, and backup evacuation plans.
Medical Complexity in Remote Settings
Our study pinpointed acute cardiovascular diseases, injuries, and musculoskeletal disorders, specifically bone fractures, as the leading causes for air medical evacuations. These conditions require rapid transport but also sophisticated medical management during evacuation.
The medical challenges extend beyond initial transport decisions. Instead, forward units will need experience providing prolonged casualty care until evacuation is possible, highlighting the importance of coordinated medical care that extends from initial response through final delivery to definitive care facilities.
Technology and Innovation in Medical Aviation
While maintaining realistic expectations about current capabilities, the medical aviation industry continues to evolve with emerging technologies. Future innovations may include:
Advancing Communication Systems
Enhanced satellite communication systems will improve coordination between evacuation teams, medical facilities, and family members, ensuring seamless information flow during critical operations.
Emerging Monitoring Technologies
Future developments in remote patient monitoring could enable real-time vital sign transmission during evacuation, allowing receiving hospitals to prepare more effectively for incoming patients.
Artificial Intelligence Applications
Technological advancements such as artificial intelligence (AI) are driving forward innovation in combat medical care, including smaller and lighter devices. Recent innovations in AI and new algorithms on hemorrhagic shock can alert medics earlier than traditional diagnostic symptoms. While these technologies are still developing for civilian applications, they represent promising future capabilities.
Unmanned Systems (Future Applications)
Currently, a NATO working group is investigating unpiloted aerial vehicles (UAVs) for casualty evacuation. While not yet operational for civilian medical evacuations, drone technology may eventually provide initial medical supply delivery or reconnaissance capabilities in extremely remote locations.
The Economic Impact of Medical Evacuation
The financial implications of medical evacuation from remote areas are significant both for individuals and healthcare systems. This study highlights the substantial economic burden associated with emergency air medical evacuations from remote islands, with cardiovascular diseases, injuries and fractures identified as major contributors.
For travelers and remote workers, understanding these costs is crucial for planning. Traditional insurance won't rescue you, and a medical evacuation can cost up to $300,000. This underscores the importance of appropriate medical evacuation insurance or membership programs for those who regularly travel to or work in remote locations.
Global Perspectives on Remote Medical Care
The challenges of remote area medical evacuation are not unique to any single country. Fig. 1 shows that the survival rate is 90% within 24 hours, 50%-60% between 25 and 48 hours, and 20%-30% between 49 and 72 hours. After 72 hours, the survival rate is 5%-10% or less. While this data relates to disaster rescue scenarios, it illustrates the critical importance of rapid response across all emergency situations.
International coordination becomes particularly important for medical evacuations that cross national borders. ParaFlight's expertise includes navigating international regulations, customs requirements, and medical certification processes that can complicate cross-border evacuations.
Case Studies in Remote Medical Evacuation Excellence
Mountain Rescue Operations
High-altitude rescues present unique challenges including weather variability, landing zone limitations, and altitude-related medical considerations. ParaFlight's coordination expertise ensures that mountain rescues consider:
- Altitude limitations for different aircraft types
- Weather pattern analysis and timing
- Specialized high-altitude medical equipment
- Coordination with local mountain rescue teams
Maritime Medical Evacuations
Ocean-based medical emergencies require specialized coordination between maritime and aviation resources. These complex operations may involve:
- Coast Guard coordination and support
- Ship-to-helicopter transfer procedures
- Extended over-water flight planning
- International waters regulatory compliance
Industrial Site Evacuations
Remote industrial operations, including mining, oil and gas, and construction sites, present unique evacuation challenges:
- Hazardous material considerations
- Limited landing zone availability
- Coordination with industrial safety teams
- Specialized trauma care requirements
Quality Assurance and Continuous Improvement
ParaFlight maintains rigorous quality assurance programs that continuously evaluate and improve evacuation outcomes. Our data-driven approach includes:
Outcome Tracking
Systematic collection and analysis of evacuation outcomes helps identify best practices and areas for improvement. This includes monitoring:
- Response times from initial contact to patient delivery
- Medical outcome measures
- Client satisfaction metrics
- Safety incident analysis
Training and Education
Ongoing education programs ensure that ParaFlight coordination teams stay current with:
- Latest medical evacuation protocols
- Regulatory changes and compliance requirements
- New aviation technologies and capabilities
- International evacuation procedures
Regulatory Framework and Compliance
The medical aviation industry operates under strict regulatory oversight designed to ensure safety and quality. Section 306 of this law directed the FAA to improve the HAA regulations, dispatching procedures, pilot training, and equipment required for Title 14 CFR Part 135 HAA operators. In April 2014, the FAA issued Final Rule RIN 2120-AJ53 entitled Helicopter Air Ambulance, Commercial Helicopter, and Part 91 Helicopter Operations.
ParaFlight's partnership approach ensures compliance with all relevant regulations while maintaining focus on medical care coordination rather than operational complexity.
Insurance and Financial Planning
Given the high costs associated with medical evacuation, proper insurance planning is essential. During the pretravel consultation, discuss insurance options and suggest that all travelers consider purchasing supplemental medical insurance coverage, particularly if they are going to remote destinations or places lacking high-quality medical facilities. Strongly encourage supplemental medical insurance coverage for travelers planning extended international travel, those with underlying health conditions, and those participating in high-risk activities (e.g., scuba diving, mountain climbing) abroad.
Comprehensive medical evacuation coverage should consider:
- Geographic coverage areas
- Maximum benefit limits
- Pre-existing condition exclusions
- Coordination with primary health insurance
- Family member transportation benefits
Future Directions in Remote Medical Evacuation
The field of remote medical evacuation continues to evolve with advances in technology, regulatory frameworks, and medical techniques. Future developments may include:
Enhanced Telemedicine Integration
Advanced telemedicine capabilities could enable real-time consultation between evacuation teams and specialist physicians, improving care during transport and preparation at receiving facilities.
Improved Weather Prediction
Better weather forecasting and real-time meteorological data could enhance flight safety and reduce weather-related delays in critical evacuations.
Expanded Network Coverage
Continued expansion of aviation infrastructure and medical facility capabilities in remote areas may reduce evacuation distances and improve access to care.
Conclusion
Rapid medical evacuation from remote areas represents one of the most challenging and critical aspects of emergency medical care. The combination of geographic isolation, weather constraints, regulatory complexity, and medical urgency requires specialized expertise and careful coordination.
ParaFlight's concierge approach addresses these challenges through expert medical coordination, exclusive partnerships with FAA-certified operators, and a commitment to safety that prioritizes patient outcomes above all else. By focusing on coordination rather than operations, ParaFlight can dedicate its expertise to what matters most: ensuring that patients in remote medical emergencies receive the rapid, safe, and appropriate care they need.
As technology continues to advance and the regulatory environment evolves, the importance of expert coordination in medical evacuation will only grow. The future of remote medical evacuation lies not just in faster aircraft or better equipment, but in the sophisticated coordination and medical expertise that transforms these tools into life-saving interventions.
For those who work, travel, or live in remote areas, understanding the realities of medical evacuation – including its costs, limitations, and requirements – is essential for proper preparation and insurance planning. When emergencies do occur, having access to expert coordination services like ParaFlight can make the difference between a successful evacuation and a tragic outcome.
The statistics are clear: The 'golden hour' medevac policy that saved the lives of US troops in Afghanistan and Iraq contributed to the best survival rates for any war in US military history. This same principle applies to civilian medical evacuations from remote areas, where expert coordination, rapid response, and appropriate medical care can literally mean the difference between life and death.
References
- Centers for Disease Control and Prevention. (2024). Travel Insurance, Travel Health Insurance & Medical Evacuation Insurance. CDC Yellow Book 2024. Available at: https://wwwnc.cdc.gov/travel/yellowbook/2024/health-care-abroad/insurance
- Hsieh, P-H., et al. (2025). Economic impact of patients with medical evacuation in remote islands: a case study in Matsu Islands. Frontiers in Public Health, 13:1542172. Available at: https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1542172/full
- Reimer, A.P. (2019). Establishing Transport Statistics: Results From the Medevac Transport Statistics Survey. Air Medical Journal, 38(4). Available at: https://www.airmedicaljournal.com/article/S1067-991X(18)30363-8/abstract
- National Association of Insurance Commissioners. Air Ambulance Insurance Coverage. Available at: https://content.naic.org/article/consumer-insight-understanding-air-ambulance-insurance-coverage

Last-Minute Jet Charter After Commercial Cancellation: Your Ultimate Solution for Emergency Travel
When commercial airlines leave you stranded with sudden cancellations, the stress can be overwhelming. Whether it's a critical business meeting, family emergency, or time-sensitive event, missing your flight can have devastating consequences. Fortunately, last-minute jet charter services provide a reliable lifeline when traditional airlines fail to deliver. This comprehensive guide explores how private jet charter can save your travel plans when commercial flights fall through.
The Reality of Commercial Flight Disruptions in 2024
Commercial aviation continues to face significant challenges with flight reliability. In 2024, 1.4% of flights were cancelled, higher than the 1.3% cancellation rate in 2023. While this might seem like a small percentage, it translates to thousands of disrupted passengers daily.
The numbers paint a concerning picture for travelers. Out of over 5 million flights in the US, around 140,000 were canceled during the observed period from March to September 2024. This leaves the US flight cancellation rate for 2024 at 2.76%. During peak periods, the situation becomes even more challenging. For July 2024, 2.9% of flights were cancelled, with the 10 marketing network carriers reporting 676,807 scheduled domestic flights, 19,574 (2.9%) of which were cancelled.
Beyond cancellations, delays create additional complications for time-sensitive travelers. Approximately 63% of all flights experienced no delay during the period studied. The majority of delays were minor, with most (around 18-22% across all months) lasting from five to 30 minutes. However, severe delays can be just as disruptive as outright cancellations.
The psychological impact on passengers is significant. Many travelers reported feeling anxious when booking travel, most commonly due to the possibility of delays or cancellations (32%), pricing issues (18%), and long waiting lines at congested airports (17%). 79% of global business travelers have experienced a travel disruption in 2023.
The Growing Private Jet Charter Market: A Reliable Alternative
The private jet charter industry has experienced remarkable growth, positioning itself as a viable solution for travelers seeking reliability and flexibility. Global Private Jets Charter Market, valued at USD 28.01 billion in 2024, will grow to USD 29.38 billion in 2025 and USD 11.9 billion by 2033, at 4.9% CAGR.
This growth reflects changing consumer priorities and expectations. There has been a 32.1% growth in private flying as compared to pre-pandemic levels in 2019, highlighting the market's robust healing and appeal. The market's resilience demonstrates its value proposition for travelers who prioritize reliability and time efficiency.
On-demand trips generated 52.18% of the private jet charter services market revenue 2024, reflecting reliance on flexible arrangements for last-minute executive travel and special events. By service model, on-demand charter held 52.18% revenue share of the private jet charter services market in 2024. This statistic underscores the importance of immediate availability for emergency and last-minute travel situations.
The demographics of private jet users are expanding beyond traditional ultra-high-net-worth individuals. By end user, corporates and SMEs secured 45.71% of demand in 2024, while sports and entertainment use is set to grow at a 9.24% CAGR to 2030. This diversification indicates that private aviation is becoming more accessible to a broader range of travelers facing urgent travel needs.
Last-Minute Travel Booking Trends: The Demand for Flexibility
Modern travelers increasingly embrace spontaneous travel decisions, creating a perfect match for on-demand charter services. Forty-four percent of leisure travelers and 56 percent of business travelers in the United States book at the last minute, and 34 percent of these travelers book a trip of 0 to 3 days in duration.
The mobile revolution has enabled this shift toward last-minute bookings. 72 percent of mobile bookings on an OTA site or through an OTA app were made within one day of the stay. About 35% of all travel bookings are now done on mobile devices.
This trend toward spontaneous travel decision-making aligns perfectly with the capabilities of private jet charter services, which can often accommodate bookings with minimal advance notice. In many cases, we can have you wheels-up in as little as 2 hours from the time of your call.
When Commercial Airlines Fail: Your Rights and Limitations
Understanding your rights when airlines cancel flights is crucial, but the reality often falls short of passenger expectations. If an airline cancels a passenger's flight or makes a significant change in the flight, regardless of the reason, airlines are required to provide a prompt refund to a ticketed passenger, including those with non-refundable tickets, should the passenger choose not to accept the alternative offered, such as rebooking on another flight.
However, Each airline has its own policies about what it will do for customers on bumped or cancelled flights. There are no federal requirements. Passengers are not entitled to direct monetary compensation under US law when a delay occurs. Instead, airlines are merely required to pay for lodging costs of passengers if the delay or a cancellation is through their own fault, but not if the cause is beyond their control, such as weather.
These limitations highlight why many travelers turn to private jet charter when commercial airlines cannot meet their travel timeline requirements. Unlike commercial airlines, charter operators can often work around weather conditions, utilize alternative airports, and provide personalized solutions that get passengers to their destinations on time.
The Strategic Advantage of Last-Minute Jet Charter
Private jet charter offers several compelling advantages when commercial flights fail to meet your needs:
Immediate Availability and Rapid Response
Private jet charter companies specialize in last-minute private jet charters that prioritize speed and discretion. In many cases, they can have you wheels-up in as little as 2 hours from the time of your call. Their rapid response charters are trusted by high-net-worth individuals, corporations, and governments.
Superior Airport Access
Private jets can access thousands more airports than commercial airlines. There are approximately 5,100 public use airports in the nation accessed by general aviation aircraft, compared to approximately 500 that offer commercial airline service. This means that business aviation reaches 10 times the number of U.S. airports than do the airlines.
This expanded airport network means you can often fly closer to your final destination, potentially saving hours of ground transportation time. When every minute counts, this accessibility advantage becomes invaluable.
Flexible Scheduling and Route Optimization
Unlike commercial airlines with fixed schedules, private jet charter allows complete scheduling flexibility. Last-minute jet charters are not only cost-effective but also offer significant flexibility. Whether it's a business emergency or a spontaneous vacation, private jets can quickly accommodate unexpected changes in travel plans. This allows for immediate departure times, ensuring you never miss out on important opportunities.
Cost-Effective Emergency Solutions
While private jet charter represents a premium travel option, it can be surprisingly cost-effective for emergency situations, especially when considering the potential costs of missed business opportunities, delayed meetings, or personal emergencies.
Booking last-minute private jet charters offers several advantages, especially for travelers with flexible schedules. These flights can result in substantial savings, particularly when passengers utilize empty-leg flights. These are unoccupied, one-way flights that provide opportunities for budget-conscious travelers seeking private travel experiences.
Types of Emergency Situations Perfect for Last-Minute Charter
Last-minute jet charter services excel in numerous emergency scenarios:
Business Emergencies
- Critical client meetings that cannot be rescheduled
- Emergency board meetings or investor presentations
- Time-sensitive deal negotiations
- Crisis management situations requiring immediate executive presence
Personal Emergencies
- Family medical emergencies
- Urgent family gatherings
- Legal proceedings requiring immediate attendance
- Educational opportunities with tight deadlines
Event-Driven Travel
- Last-minute invitations to exclusive events
- Emergency speaker replacements at conferences
- Sports events and entertainment opportunities
- Weather-related rerouting for important occasions
Spontaneous travel often requires last-minute private jet bookings, offering unmatched flexibility and convenience. This makes private aviation ideal for attending urgent family gatherings, critical business meetings, or reacting to unforeseen invitations. Private jets allow for the quick adaptation of travel plans, crucial in emergencies or last-minute business opportunities.
The ParaFlight Advantage: FAA-Certified Excellence in Emergency Charter
When selecting a last-minute charter service, partnering with a company that exclusively works with FAA-certified operators ensures the highest safety standards and reliability. ParaFlight's concierge model provides expert guidance through every aspect of your emergency travel needs, from aircraft selection to ground transportation coordination.
Our network of FAA-certified operators maintains rigorous safety standards while delivering the flexibility and responsiveness required for emergency travel situations. Unlike booking platforms or direct ownership models, our expert-driven approach ensures that every flight is optimized for your specific emergency requirements.
We understand that emergency travel situations require immediate attention and flawless execution. Our team's expertise in navigating complex scheduling challenges, weather considerations, and regulatory requirements ensures that your urgent travel needs are met with professionalism and reliability.
Market Growth and Future Trends
The private jet charter industry's growth trajectory indicates increasing recognition of its value for emergency and time-sensitive travel. The global business jet market size was valued at USD 46.51 billion in 2024. The market is anticipated to grow from USD 48.13 billion in 2025 to USD 67.68 billion by 2032, exhibiting a CAGR of 4.99% during the forecast period.
The Global Private Aircraft Market size is expected to be worth around USD 80.8 Billion By 2034, from USD 26.6 billion in 2024, growing at a CAGR of 6.7% during the forecast period from 2025 to 2034.
This growth is driven by increasing recognition of private aviation's value proposition for time-sensitive travel. The private jet industry is experiencing significant growth in 2024, surpassing pre-pandemic levels. Growth is driven by increased wealth, pandemic concerns, business travel needs, and desire for better experiences.
Technology and Innovation in Emergency Charter Services
The industry continues to evolve with technological innovations that enhance the last-minute booking experience. Additionally, the adoption of digital platforms and artificial intelligence is streamlining reserving processes, making personal aviation more reachable. Technological advancements and virtual booking platforms have further streamlined the private jet charter industry, making access to simpler for broader purchasers.
While artificial intelligence and advanced booking platforms represent exciting future innovations, current technology already enables rapid aircraft sourcing, real-time availability checking, and streamlined booking processes that can accommodate emergency travel needs within hours of initial contact.
Regional Market Dynamics and Accessibility
In 2024, North America maintained a dominant position in the private aircraft market, securing more than a 45% share with revenues amounting to USD 11.97 billion. North America boasts a mature aviation infrastructure and a high concentration of high-net-worth individuals who drive demand for private aircraft for both personal and business travel.
This mature infrastructure provides significant advantages for emergency charter situations, with extensive maintenance facilities, training centers, and airport networks capable of supporting rapid-response charter operations.
The concentration of charter operators and aircraft availability in major business centers ensures that emergency travel needs can often be accommodated with minimal positioning time and costs.
Maximizing Value in Emergency Charter Situations
When facing a commercial airline cancellation, several strategies can optimize your charter experience:
Timing Considerations
Although last-minute private jet deals can help save time and money, it's essential to consider potential increased costs during high-demand periods like holidays. Reduced aircraft availability during these times can drive prices up. However, proximity to the private aircraft plays a key role in determining costs; booking in advance can help secure a nearby jet, thus minimizing repositioning expenses.
Flexibility in Aircraft Selection
Being open to different aircraft types and sizes can significantly improve availability and pricing for emergency charter needs. Light jets may be perfectly suitable for short-distance emergency travel, while longer trips may require mid-size or heavy jets.
Alternative Airport Considerations
The vast network of airports accessible to private jets provides numerous options for optimizing your travel route and timeline. Your charter advisor can identify alternative airports that may offer better positioning, reduced congestion, or more convenient ground transportation options.
Planning for the Unexpected: Building Charter Relationships
While emergency charter services excel at handling unexpected situations, establishing relationships with reputable charter providers before you need them offers significant advantages. Pre-qualifying operators, understanding pricing structures, and having contact information readily available can dramatically reduce response times when emergencies arise.
Consider developing contingency travel plans that include charter options for critical business travel or family situations. This proactive approach ensures that when commercial airline cancellations threaten important plans, you have immediate access to reliable alternatives.
Conclusion: Turning Travel Crises into Opportunities
Commercial flight cancellations don't have to derail your important plans. The growing private jet charter industry, driven by increasing demand for flexibility and reliability, offers a proven solution for emergency travel needs. With same-day booking capabilities, access to thousands of airports, and personalized service that addresses your specific requirements, last-minute charter services transform travel crises into manageable situations.
The statistics clearly demonstrate both the ongoing challenges with commercial aviation reliability and the robust growth of the private jet charter industry. As more travelers recognize the value of guaranteed departure times, flexible scheduling, and personalized service, charter aviation continues to evolve as an essential component of modern business and personal travel strategies.
When your next commercial flight gets canceled, remember that ParaFlight's network of FAA-certified operators stands ready to provide the reliable, safe, and efficient transportation solution you need. Our expert-driven approach ensures that your emergency travel situation receives the immediate attention and professional execution required to get you to your destination on time.
Don't let airline cancellations control your schedule. Take control with last-minute jet charter services that prioritize your time, safety, and peace of mind.
References
- U.S. Department of Transportation - Air Travel Consumer Report: December 2024, Full Year 2024 Numbers
- TravelPerk - 2024 delayed and canceled flight trends & stats
- Business Research Insights - Private Jets Charter Market Size
- Peek Pro - Last-Minute Travel Booking Trends
- U.S. Department of Transportation - Airline Cancellation and Delay Dashboard

Private Aviation Preparedness and Protocols During Natural Disasters: Your Complete Emergency Response Guide
When natural disasters strike, traditional transportation networks often become overwhelmed or completely inaccessible. Commercial airlines ground flights, highways become impassable, and emergency services reach capacity. In these critical moments, private aviation emerges as a vital lifeline for evacuations, medical emergencies, and disaster relief operations. Understanding the preparedness protocols and emergency response capabilities of private aviation can mean the difference between safety and danger during catastrophic events.
The Growing Role of Private Aviation in Disaster Response
Natural disasters have become increasingly frequent and severe in recent years. Hurricane Helene in 2024 became the most recent hurricane to impact South Carolina, causing a statewide event with 21 tornadoes, downed trees, and widespread power outages. Other hurricanes that have affected the Palmetto State in recent years include Hurricane Matthew in 2016, Hurricane Irma in 2017, Hurricane Florence in 2018, Hurricane Dorian in 2019, Hurricane Ian in 2022, Hurricane Idalia in 2023, and Hurricane Debby in 2024. Each of these events demonstrated the critical importance of having robust emergency transportation alternatives when conventional systems fail.
The fastest-growing segment in the jet charter industry involves medical evacuation, with this market growing at 7.5% CAGR. Medivac growth is driven by factors like climate change, which increases the risk of natural disasters and associated medical emergencies. The private aviation industry has evolved beyond luxury travel to become an essential component of emergency response infrastructure.
Medical evacuation can be the difference between life and death during natural disasters, and private jet charters have significantly enhanced the capabilities and efficiency of these operations compared to traditional medivac services. The flexibility and speed of private aircraft make them invaluable assets during crisis situations.
Pre-Disaster Planning: The Foundation of Effective Response
Establishing Emergency Response Protocols
Effective disaster preparedness in private aviation begins long before storm clouds appear on the horizon. Platinum-rated operators must have a Safety Management System and Emergency Response Plan in place, along with documented operations and maintenance standards and records. These comprehensive plans serve as the blueprint for coordinated response efforts during emergencies.
Professional aviation service providers work exclusively with FAA-certified operators who maintain rigorous preparedness standards. This certification process ensures that operators meet stringent federal requirements for aircraft maintenance, pilot qualifications, and emergency procedures. The importance of this certification cannot be overstated. It represents the difference between reliable emergency services and potentially dangerous operations during crisis situations.
Pre-Planning and Risk Assessment
Pre-planning components include 24/7 global air evacuation planning and implementation services, with evacuations carried out based on pre-planning with preferred aircraft access and transfers to pre-selected destinations. This advance preparation is crucial because decisions made under pressure during emergencies rarely match the quality of those made during calm planning periods.
Risk assessment involves analyzing potential disaster scenarios specific to geographic regions. For coastal areas, hurricane preparedness takes priority, while regions prone to wildfires, earthquakes, or severe winter weather require different protocols. Each scenario demands specific aircraft capabilities, routing plans, and coordination procedures with local emergency management authorities.
Documentation and Regulatory Compliance
All necessary documentation, including passports and visas, must be prepared to ensure safe entry into foreign countries, as standard immigration rules apply even during crises. Companies should take proactive measures to ensure documentation is in place before disaster seasons begin. This preparation extends beyond individual travel documents to include aircraft registration, insurance certificates, and operational authorizations for international flights.
During-Disaster Response Protocols
Critical Timing Considerations
Evacuation decisions should be considered 72 hours or more prior to a storm's arrival, as there is a limited window of opportunity after this timeframe. Once winds reach excess of 30 mph, evacuation may no longer be feasible due to aircraft landing limitations. This narrow operational window underscores the importance of proactive decision-making and rapid response capabilities.
The physics of flight operations create inflexible safety parameters that cannot be compromised, regardless of urgency. Aircraft have specific wind limitations for takeoff and landing operations, and these limits are non-negotiable. Understanding these constraints helps emergency planners make realistic timing decisions and communicate accurate expectations to those requiring evacuation services.
Coordination with Federal Aviation Administration
During natural disasters, awareness of active Temporary Flight Restrictions (TFRs) and updates to Notices to Airmen (NOTAMs) is vital, as these can change rapidly during emergency response efforts. We strongly recommend that you receive real-time flight updates through your electronic flight planning tools (EFP) or use VFR Flight Following. The FAA plays a central coordinating role in managing airspace during disasters, ensuring that emergency response aircraft can operate safely while maintaining overall system integrity.
Any TFRs established by the FAA include instructions on restrictions and identify who can operate in affected airspace. NOTAMs for restrictive TFRs provide contact numbers for access requests, though pre-coordination with Florida and Federal air operations officials at State Emergency Operations Centers is preferred. This coordination process ensures that legitimate emergency flights receive priority while maintaining safety standards.
Multi-Agency Coordination During Response
During Hurricane Katrina, Operation AIR CARE provided emergency airlift support to more than 24,000 New Orleans residents through coordination between the Air Transport Association, FAA, and FEMA. U.S. and foreign commercial carriers along with military aircraft provided substantial resources. This massive coordinated effort demonstrated the scalability of aviation response when properly organized.
The success of such operations depends on clear communication channels between private operators, government agencies, and emergency management officials. Each entity brings specific capabilities and resources, but coordination prevents duplication of efforts and ensures optimal use of available aircraft and personnel.
FAA Certification and Safety Standards
Operator Certification Requirements
Private jets must adhere to stringent certification standards set by the FAA, encompassing structural integrity, engine performance, and safety features. This certification ensures that every private jet meets the highest levels of safety and performance before taking to the skies through a rigorous process that guarantees passenger safety and aircraft reliability.
The certification process extends far beyond initial aircraft approval. Regular maintenance and rigorous inspection are key components of private jet operations, ensuring that every component from engines to electronics is in top working condition through scheduled maintenance checks and unexpected repairs as part of ongoing processes to maintain high FAA safety standards.
Pilot Qualifications and Training
Pilots operating private jets are highly trained professionals with extensive training, certification, and regular skill assessments. They are trained to handle various situations, from adverse weather conditions to emergency scenarios, ensuring that private jet pilots are among the best in the aviation industry.
Professional operators require a minimum of two FAA-certified, ATP-rated pilots on every flight, with minimum experience requirements significantly higher than FAA or industry standards. These minimums include certified hours flying specific aircraft types for both command pilots and second-in-command, with verification of crew credentials, aircraft insurance, and operations certificates before every flight.
Safety Management Systems
Professional operators maintain certifications that reflect strict adherence to industry-leading safety standards and protocols, partnering with vetted operators who meet FAA and international safety standards while prioritizing pilot qualifications, conducting regular aircraft maintenance, and implementing safety management systems.
The safety management approach involves continuous monitoring, reporting, and improvement of operational procedures. This systematic approach identifies potential risks before they become actual safety hazards and ensures that lessons learned from incidents are incorporated into updated procedures.
Technology and Emergency Communication Systems
Current Communication Capabilities
Real-time flight updates through electronic flight planning tools (EFP) and VFR Flight Following provide essential information during emergency operations. These systems ensure that emergency flights maintain continuous communication with air traffic control and emergency coordination centers.
Modern aircraft are equipped with multiple communication systems providing redundancy during critical operations. Satellite communication systems maintain connectivity even when ground-based infrastructure is damaged or overwhelmed. This capability proves essential when coordinating complex multi-aircraft evacuation operations or providing real-time updates to emergency management officials.
Medical Emergency and Evacuation Protocols
Medical Transport Capabilities
During the COVID-19 pandemic, private jets transported critically ill patients to specialized care facilities across borders, often within hours of receiving calls. In natural disaster scenarios such as earthquakes or hurricanes, private jets evacuate injured individuals from areas otherwise inaccessible due to damaged infrastructure.
The medical transport capability extends beyond simple patient transport. Arranging medivac flights involves medical assessment to determine patient condition and required care during flight, with adherence to stringent regulatory standards including compliance with international aviation laws, certification of medical staff and equipment, and regular maintenance checks of aircraft meeting specific safety standards set by aviation authorities.
Specialized Equipment and Personnel
Medical evacuation flights require specialized equipment and trained medical personnel capable of providing advanced life support during transport. The aircraft must be configured with appropriate medical equipment, and the flight crew must be trained in medical transport procedures. This specialization requires additional certification and training beyond standard commercial operations.
The coordination between medical teams, aircraft operators, and receiving facilities requires precise timing and communication. Medical emergencies during disasters often involve multiple patients, requiring coordination of multiple aircraft and medical teams to ensure optimal patient outcomes.
Regional Considerations and Disaster Types
Hurricane and Coastal Storm Preparedness
Hurricane season begins June 1 and lasts through November 30, creating a defined period when coastal regions must maintain heightened preparedness. During Category 5 Hurricane Dorian in 2019, professional operators swiftly evacuated hundreds of stranded travelers, and following Hurricanes Irma and Maria in 2017, coordinated chartered evacuation flights across the Caribbean while delivering critical aid and relief supplies.
The Caribbean region presents unique challenges due to limited infrastructure and the vulnerability of small island nations to complete isolation during major storms. Private aviation provides the only viable evacuation option when commercial airlines suspend operations and sea transport becomes impossible.
Geographic Risk Factors
Certain regions, notably Alaska and mountainous states in the northwestern US, exhibit higher accident rates due to challenging operating conditions. In Alaska, only 18% of communities are accessible by road, leading to higher reliance on aviation and increased exposure to potential accidents. These statistics highlight the varying risk profiles across different geographic regions.
Understanding regional characteristics helps emergency planners develop appropriate response strategies. Mountain regions require aircraft capable of high-altitude operations, while coastal areas need aircraft that can operate from shorter runways that may be partially damaged by storm surge or flooding.
Economic Considerations and Resource Planning
Cost Factors During Emergencies
Due to emergency conditions, many experience challenges with scarce flight options. During natural disasters, private jet availability becomes even more limited due to high demand, with charter pricing increasing quickly as storms approach and conditions worsen, as aircraft and airports become more limited.
The economic reality of emergency aviation services requires advance planning and realistic budgeting. Emergency pricing reflects the increased risks, limited availability, and urgent timing requirements inherent in disaster response operations. Organizations and individuals who pre-plan and establish relationships with certified operators often secure better availability and more predictable pricing during emergencies.
Insurance and Liability Considerations
Emergency operations involve elevated risks that must be properly insured and managed. Aircraft operators must maintain appropriate insurance coverage for emergency operations, and passengers should understand their coverage limitations during crisis situations. The legal and financial complexities of international emergency evacuations require careful advance planning to avoid complications during actual emergencies.
ParaFlight's Concierge Approach to Emergency Preparedness
As a concierge service specializing in private aviation coordination, ParaFlight serves as the crucial link between clients and FAA-certified operators during emergency situations. Our expert-driven model focuses on advance planning, rapid response coordination, and seamless execution of emergency transportation requirements.
Our team maintains relationships with certified operators across multiple regions, ensuring availability during crisis situations when individual operators may be overwhelmed or unavailable. This network approach provides redundancy and options that individual operator relationships cannot match.
The concierge model proves particularly valuable during emergencies because it eliminates the need for clients to research operators, verify certifications, and coordinate complex multi-leg evacuations under pressure. Our expertise in regulations, routing, and logistics allows clients to focus on safety and decision-making while we handle operational complexities.
Best Practices for Emergency Preparedness
Advance Planning Recommendations
Effective emergency preparedness requires advance planning during non-emergency periods. This planning should include identifying potential evacuation destinations, understanding documentation requirements, and establishing communication protocols with family members and business associates. The stress and time pressure of actual emergencies make clear advance planning essential.
Regular review and updating of emergency plans ensures they remain current with changing circumstances, regulations, and personal situations. Plans developed years ago may no longer reflect current family situations, business requirements, or regulatory environment.
Communication Protocols
Establishing clear communication protocols ensures that all parties understand their roles and responsibilities during emergencies. These protocols should include primary and backup communication methods, designated decision-makers, and procedures for updating plans as situations evolve.
The communication plan must account for potential infrastructure damage that may affect normal communication systems. Satellite phones and other backup communication methods may become necessary during major disasters.
Regulatory Compliance and Documentation
International Considerations
Emergency evacuations often involve international flights, bringing additional regulatory complexity. Challenges include navigating international airspace regulations, language barriers, and coordinating between multiple healthcare systems, though private jet charters help address these challenges by offering flexible and controlled transportation options.
Advance preparation of international documentation prevents delays during actual emergencies. This preparation includes ensuring passport validity, obtaining necessary visas for potential destination countries, and understanding customs and immigration procedures for emergency entries.
Record Keeping and Reporting
Emergency operations require careful documentation for regulatory compliance, insurance claims, and post-event analysis. Operators must maintain detailed records of flight operations, passenger manifests, and coordination with government agencies. This documentation serves multiple purposes and may be required for regulatory review or insurance claims processing.
Future Developments and Industry Trends
Industry Growth and Capacity
The jet charter industry was worth $21.24 billion in 2024 and is expected to grow to $24.28 billion in 2025, indicating expanding capacity and capabilities that may benefit emergency response operations. This growth suggests increasing availability of aircraft and operators, potentially improving response capabilities during disasters.
The expansion of the private aviation industry provides additional resources for emergency operations, but also increases the importance of proper vetting and certification verification. Not all operators meet the same safety standards, making professional coordination services more valuable.
Conclusion
Private aviation serves as a critical component of modern disaster response infrastructure, providing capabilities that complement and extend traditional emergency services. The effectiveness of these services depends on proper advance planning, coordination with certified operators, and understanding of regulatory requirements and operational limitations.
The protocols and preparedness measures outlined in this guide represent current best practices based on lessons learned from recent disaster response operations. As natural disasters become more frequent and severe, the importance of understanding and utilizing private aviation emergency capabilities will only increase.
Success in emergency aviation operations requires the coordination of multiple specialized entities: FAA-certified operators provide the aircraft and crews, government agencies manage airspace and regulatory compliance, and professional coordination services like ParaFlight bridge the gap between emergency needs and available resources.
The time to plan for aviation emergency services is before emergencies occur. Advance planning, relationship building, and understanding of capabilities and limitations ensure that when disasters strike, private aviation can provide the rapid, flexible response that may prove essential for safety and survival.
By working exclusively with FAA-certified operators and maintaining rigorous safety standards, the private aviation industry continues to evolve as a reliable resource for emergency transportation when traditional systems become overwhelmed or unavailable. The investment in proper emergency preparedness pays dividends when crisis situations arise and rapid, safe transportation becomes a matter of life and death.
References
- Federal Aviation Administration. (2024). Severe Weather and Natural Disaster Preparedness. Retrieved from FAA.gov
- National Business Aviation Association. (2022). Emergency Response. Retrieved from NBAA.org
- International Civil Aviation Organization. (2024). Emergency Response Planning. Retrieved from ICAO.int
- South Carolina Emergency Management Division. (2024). Hurricane Preparedness Month. Retrieved from SCEMD.org

Introducing Air Nurses x ParaFlight: In-Flight Medical Care, Redefined
Expert Care, In Flight
At ParaFlight, we are proud to offer an exclusive service that goes beyond traditional private jet charters by partnering with Air Nurses, a concierge flight nursing service designed specifically for luxury medical transport in private aviation. Together, we provide a seamless and elevated in-flight medical experience, ensuring that comfort and medical expertise go hand-in-hand throughout the entire journey.
.png)
Who Is Air Nurses?
Air Nurses is a luxury concierge medical service offering board-certified flight nurses who provide comprehensive in-flight medical care. Founded by Ericka Essington BSN, RN, NRP, CFRN, FP-C, CMTE with over 15 years of experience in critical care transport and aviation medicine. Air Nurses have set the bar for medical oversight in private aviation. With Air Nurses, you have a team of elite, aviation-experienced professionals who are solely dedicated to providing medical care and peace of mind during the flight. They come on board your flight as additional crew, seamlessly integrating with your team to ensure continuous medical oversight throughout the journey.
Whether assisting with post-surgical recovery, managing chronic conditions, supporting elderly and pediatric travelers, or offering care for individuals with cognitive needs or those requiring additional support during recovery and wellness transitions, Air Nurses delivers a calm, capable presence onboard, ensuring seamless continuity and comfort from the moment you leave the ground to your final destination.
How Air Nurses Elevates ParaFlight’s Services
• In-Flight Medical Expertise: Air Nurses provide expert medical care aboard private jets, ensuring clients receive real-time monitoring, medication management, and mobility assistance, all while maintaining the highest standard of care. This clinical oversight guarantees that clients with complex medical needs travel safely and comfortably.
• Tailored Medical Solutions: Air Nurses offer customized solutions for each individual flight. From personalized medications and medical equipment to specific care protocols, Air Nurses ensure that every need is anticipated and addressed before departure, allowing clients to travel with confidence.
• Door-to-Destination Care: Air Nurses provide seamless, door-to-destination care, from bedside-to-aircraft transfers to arrival at the destination, ensuring continuous care throughout the entire journey.
• Coordinated Care: Air Nurses work in tandem with ParaFlight and any relevant physicians, family offices, and destination teams, making sure the journey is as smooth and efficient as possible. This seamless coordination enhances the overall experience, ensuring that all aspects of the trip, medical and logistical.are perfectly aligned.
• Luxury and Precision: By adding Air Nurses to ParaFlight’s suite of services, we deliver not only luxury aviation but also peace of mind for travelers with medical needs. This seamless integration of luxury aviation and medical care provides clients with a solution that meets both their comfort and health needs.
A New Class of Medically Supported Travel
Air Nurses and ParaFlight are elevating the standard for in-flight medical care, offering a refined alternative built specifically for private aviation. Every mission combines clinical expertise with seamless charter execution, delivering calm, comfort, and continuity at altitude.
Let’s Build the Mission Around You
For tailored itineraries and onboard medical support, contact our team 24/7:
📧 info@paraflight.aero
📞 1-844-538-1911 (Immediate Assistance)

Introducing Air Nurses x ParaFlight: In-Flight Medical Care, Redefined
Expert Care, In Flight
At ParaFlight, we are proud to offer an exclusive service that goes beyond traditional private jet charters by partnering with Air Nurses, a concierge flight nursing service designed specifically for luxury medical transport in private aviation. Together, we provide a seamless and elevated in-flight medical experience, ensuring that comfort and medical expertise go hand-in-hand throughout the entire journey.
.png)
Who Is Air Nurses?
Air Nurses is a luxury concierge medical service offering board-certified flight nurses who provide comprehensive in-flight medical care. Founded by Ericka Essington BSN, RN, NRP, CFRN, FP-C, CMTE with over 15 years of experience in critical care transport and aviation medicine. Air Nurses have set the bar for medical oversight in private aviation. With Air Nurses, you have a team of elite, aviation-experienced professionals who are solely dedicated to providing medical care and peace of mind during the flight. They come on board your flight as additional crew, seamlessly integrating with your team to ensure continuous medical oversight throughout the journey.
Whether assisting with post-surgical recovery, managing chronic conditions, supporting elderly and pediatric travelers, or offering care for individuals with cognitive needs or those requiring additional support during recovery and wellness transitions, Air Nurses delivers a calm, capable presence onboard, ensuring seamless continuity and comfort from the moment you leave the ground to your final destination.
How Air Nurses Elevates ParaFlight’s Services
• In-Flight Medical Expertise: Air Nurses provide expert medical care aboard private jets, ensuring clients receive real-time monitoring, medication management, and mobility assistance, all while maintaining the highest standard of care. This clinical oversight guarantees that clients with complex medical needs travel safely and comfortably.
• Tailored Medical Solutions: Air Nurses offer customized solutions for each individual flight. From personalized medications and medical equipment to specific care protocols, Air Nurses ensure that every need is anticipated and addressed before departure, allowing clients to travel with confidence.
• Door-to-Destination Care: Air Nurses provide seamless, door-to-destination care, from bedside-to-aircraft transfers to arrival at the destination, ensuring continuous care throughout the entire journey.
• Coordinated Care: Air Nurses work in tandem with ParaFlight and any relevant physicians, family offices, and destination teams, making sure the journey is as smooth and efficient as possible. This seamless coordination enhances the overall experience, ensuring that all aspects of the trip, medical and logistical.are perfectly aligned.
• Luxury and Precision: By adding Air Nurses to ParaFlight’s suite of services, we deliver not only luxury aviation but also peace of mind for travelers with medical needs. This seamless integration of luxury aviation and medical care provides clients with a solution that meets both their comfort and health needs.
A New Class of Medically Supported Travel
Air Nurses and ParaFlight are elevating the standard for in-flight medical care, offering a refined alternative built specifically for private aviation. Every mission combines clinical expertise with seamless charter execution, delivering calm, comfort, and continuity at altitude.
Let’s Build the Mission Around You
For tailored itineraries and onboard medical support, contact our team 24/7:
📧 info@paraflight.aero
📞 1-844-538-1911 (Immediate Assistance)